The Screening: Brain MRI and The Bern Score
The diagnostic pathway starts with a Brain MRI. Radiologists often use the SEEPS acronym: Subdural fluid collections, Enhancement of pachymeninges, Engorgement of venous structures, Pituitary hyperemia, and Sagging of the brain. These signs are helpful, but they are qualitative and vary between cases.
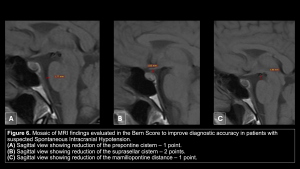
To improve accuracy, we use the Bern Score, a semi-quantitative system (range 0–9) that predicts spinal CSF leak. It is based on six MRI criteria (Dobrocky et al., JAMA Neurol. 2019).
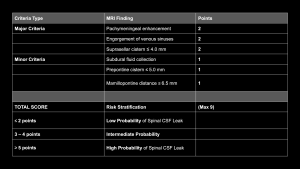
Calculated on T1-weighted sequences (contrast-enhanced for dural signs; mid-sagittal for metric measurements), the criteria are:
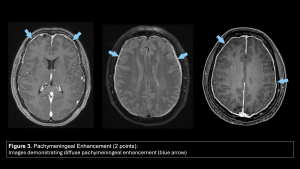
- Pachymeningeal Enhancement (2 points):
- Positive: Smooth, continuous, non-nodular enhancement of the dura mater (sparing the leptomeninges). This is the most common sign, but it can be absent in chronic cases.
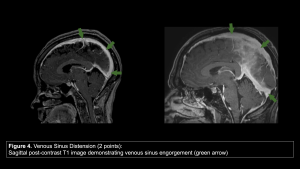
- Engorgement of venous sinuses (2 points): Assessed at the dominant transverse sinus on lateral slices.
- Positive: Change from the normal oval/flat cross-section to a rounded, distended appearance due to compensatory venous pooling.
- Suprasellar Cistern Height (2 point): Measured on the mid-sagittal plane.
- Positive: Height ≤ 4.0 mm.
- Mechanism: Downward traction of the brainstem obliterates the cistern.
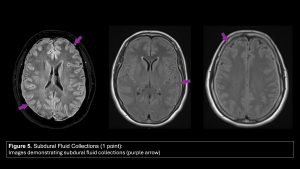
- Subdural Fluid Collections (1 point):
- Positive: Presence of bilateral subdural hygromas (fluid signal similar to CSF).
- Prepontine Cistern Width (1 point): Measured on the mid-sagittal plane at the level of the pons midpoint.
- Positive: Width ≤ 5.0 mm.
- Mechanism: The pons is flattened against the clivus ("belly-flat sign").
- Mamillopontine Distance (1 point): Measured on the mid-sagittal plane as the shortest distance between the inferior aspect of the mammillary bodies and the superior aspect of the pons.
- Positive: Distance ≤ 6.5 mm.
- Mechanism: Inferior displacement of the hypothalamus and mesencephalon.
Score Interpretation and Probability of Spinal CSF Leak:
Low Probability (Score ≤ 2): < 10% likelihood. Search for alternative diagnoses.
Intermediate Probability (Score 3–4): Indeterminate. Clinical correlation is essential.
High Probability (Score ≥ 5): > 80% likelihood of a spinal CSF leak. Proceed directly to specialized myelography.
The Hunt: Myelography Protocol
The Challenge
Why Conventional Imaging Fails: Unlike dural tears, CSF-venous fistulas shunt CSF directly into the systemic circulation and rarely cause fluid to collect in the epidural space. Therefore, conventional spine MRI is usually negative. It does not show the hyperintense epidural signal used to identify dural defects. Standard prone myelography often fails to detect CVFs because gravity pulls the contrast ventrally, away from the dorsal nerve root sleeves where most fistulas originate.
The Game Changer
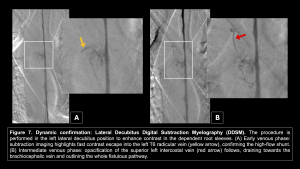
Lateral Decubitus Positioning: The key procedural change is positioning the patient laterally. Gravity pools contrast over the lateral nerve roots, forcing them into the fistula.
- Impact: This manoeuvre has been shown to increase contrast attenuation within the draining vein by over 500%.
- Yield: Decubitus positioning improves the diagnostic yield approximately 5-fold compared to prone positioning (rising from ~15% to ~74%)
Digital Subtraction Myelography (DSM)
Catching the Flow: DSM is the preferred screening modality due to its superior temporal resolution.
- Dynamic Visualization: It enables real-time detection of rapid CSF flow into the venous system.
- Background Suppression: Digital subtraction eliminates osseous noise, revealing the subtle "flash" of contrast escaping the nerve root, which might be obscured on non-subtracted images.
CT Myelography (CTM)
The "Hyperdense Paraspinal Vein" Sign: On CTM, the confirmatory finding is the "Hyperdense Paraspinal Vein" sign. This represents a contrast extending directly from the subarachnoid space into the venous system.
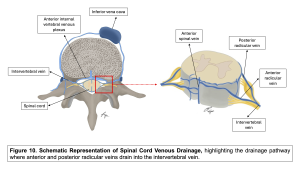
- Anatomy: Approximately 82% of fistulas arise from a nerve root sleeve diverticulum.
- What to look for: Look for contrast opacifying a tubular segmental vein or, more subtly, the internal vertebral venous plexus (IVVP), which may appear as a fine reticular network or crescentic density in the epidural space.
Pitfalls and Interpretation
The "Normal Spine" Trap (The False Negative)
The most significant pitfall in diagnosing CVFs is relying on conventional MRI markers of the spine.
- The Trap: Radiologists typically search for extrathecal fluid collections. However, CVFs shunt CSF directly into the venous system, bypassing the epidural space. Consequently, spine MRI is often completely normal.
- The Lesson: A normal spine MRI does not exclude a CSF leak. If the Brain MRI/Bern Score suggests SIH, dynamic myelography is warranted, even in the absence of spinal fluid collections.
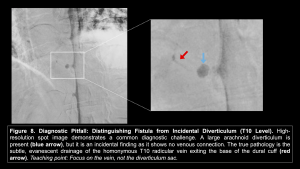
The Diverticulum Dilemma (The False Positive)
Meningeal diverticula are ubiquitous, but identifying the "culprit" requires strict criteria.
- The Trap: Assuming a large nerve root diverticulum is the leak source simply because it is prominent.
- The Lesson: A diverticulum is only a fistula if it demonstrates early venous drainage. A contrast-filled sac without an exiting hyperdense vein is merely an incidental diverticulum.
The "Cistern Measurement" Bias
While the Bern Score is a powerful tool, recent data highlights the risk of over-reliance on quantitative measurements alone.
- The Trap: Diagnosing SIH based solely on reduced cistern measurements (e.g., prepontine ≤5mm) in patients with equivocal symptoms.
- The Evidence: Kang et al. (2025) demonstrated that 22% of normal patients (without SIH) have an intermediate Bern Score (3-4 points) driven exclusively by reduced cistern dimensions.
- The Lesson: Cistern effacement is not specific in isolation. Intermediate scores require corroboration with qualitative signs (venous engorgement, pachymeningeal enhancement) or strong clinical suspicion.
The Cure: Endovascular Management
Targeted Embolization
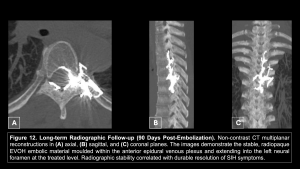
Once the fistula is localized, transvenous embolization with liquid embolic agents (e.g., Onyx/EVOH) offers a minimally invasive alternative to surgical ligation. The goal is to occlude the connection between the venous pouch and the paraspinal vein while preserving the drainage of the spinal cord.
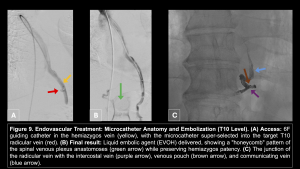
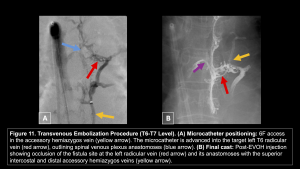
Outcomes and Follow-up
Successful occlusion is defined by the penetration of the embolic agent into the proximal radicular vein and the adjacent internal vertebral venous plexus. Post-procedural imaging confirms the stability of the embolic cast.