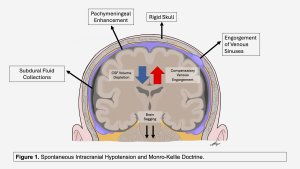
Spontaneous intracranial hypotension is a condition of CSF volume loss. This fits the Monro-Kellie hypothesis: in a closed system, CSF loss is balanced by an increase in the venous compartment. This process leads to classic brain MRI findings: venous engorgement, pachymeningeal enhancement, pituitary hyperemia, and subdural fluid collections.
A paradigm shift has occurred with the Schievink classification. Unlike ventral dural tears (Type 1 leaks) and leaking meningeal diverticula (Type 2 leaks), which usually cause spinal longitudinal extradural fluid on MRI, CSF-venous fistulas (Type 3 leaks) are direct, abnormal connections between the subarachnoid space and nearby paraspinal veins, allowing CSF to flow freely into the systemic circulation.
The Clinical Problem: CVFs rarely result in fluid accumulation in the epidural space. As a result, patients have severe orthostatic headaches, but the spine MRI often appears normal. This leads to missed diagnoses in patients with no obvious epidural leaks. High clinical suspicion and advanced myelographic techniques are needed for detection.