The main revisions in the 6th edition are summarized in four key points: 1) the addition of the section “Recommendations for Low-Dose CT Lung Cancer Screening in Japan”; 2) the change in the recommended solid component diameter for a definitive diagnosis in part-solid nodules with a total mean diameter of less than 15 mm from ≥5 mm to ≥8 mm; and the follow-up observation for nodules with a total mean diameter of less than 15 mm and a solid component diameter of less than 8 mm is now recommended at 3, 6, 12, 24, 36, 48, and 60 months; 3) the replacement of the suggested case images; and 4) the introduction of the standards of the Lung Cancer CT Screening Certification Organization
1. Recommendations for Low-Dose CT Lung Cancer Screening in JapanThe effectiveness of low-dose CT lung cancer screening has recently been demonstrated in several large-scale randomized controlled trials in Europe and the USA. According to these results, the Japanese Lung Cancer Society has issued the Lung Cancer Screening Guidelines 2022, with recommendation grades for low-dose CT lung cancer screening published online.
2. Guidelines for the Management of Pulmonary Nodules Detected by Low-Dose CT Lung Cancer Screening
Schema of the 6th edition of this guideline is shown in Figure 1.
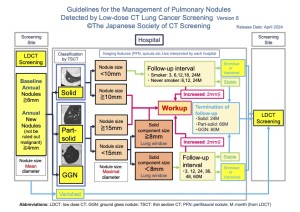
2-1. Role of Screening Institutions (left side in Figure 1)
For pulmonary nodules identified on screening CT images, the criterion for referral to specialized medical institutions for further examination is based on the average of the maximum and minor diameters. If the average size of the pulmonary nodules is less than 6 mm, a follow-up CT examination after 12 months is recommended.
For newly appearing nodules measuring 4mm or more where the possibility of lung cancer cannot be ruled out, patients will be referred to a medical institution if further examination is deemed necessary.
2-2. Role of Further Examination Medical Institutions (center in Figure 1)
At further examination medical institutions, the size criterion is determined by the maximum diameter observed on initial TS-CT scans. Pulmonary nodules with a maximum diameter of 6 mm or more are classified into solid nodules, part-solid nodules, and ground-glass nodules
- Solid Nodules (Figures 2-5)
On TS-CT, solid nodules with a maximum diameter of 10 mm or more are basically recommended workup for definitive diagnosis. For solid nodules with a maximum diameter between 6 mm and <10 mm, smokers are recommended to observe over intervals of 3, 6, 12, 18, and 24 months on TS-CT. Meanwhile, nonsmokers are recommended to observe at intervals of 6, 12, and 24 months. In both cases, i) if an increase of 2 mm or more in the maximum nodule diameter is observed, workup for definitive diagnosis is recommended. ii) If the nodule remains unchanged over two years, follow-up on TS-CT could be terminated, and these cases are recommended to referr back to the screening institution. iii) If nodule shrinkage or vanishing is observed during follow-up, these cases could be to return to the screening institution for further screening CT evaluation.


- Part-Solid Nodules (Figures 6, 7)
Part-solid nodules, which are more likely to represent malignant disease, necessitate confirmation of any reduction or disappearance on TS-CT after 3 months, because inflammatory lesions are also seen as part-solid nodules on TS-CT. If the nodule with total maximum diameter exceeds 15 mm, a definitive diagnosis is pursued (Figure 6).
For nodules with a total maximum diameter of less than 15 mm, if the maximum diameter of the solid component measures 8 mm or more at lung window setting on TS-CT, a definitive diagnosis is conducted. Meanwhile, if the solid component measures less than 8 mm, follow-up observation is recommended. This revision has adopted 8 mm as the threshold, aligning with Lung-RADS™ and several recent studies suggesting that a solid component diameter of 8 mm at lung window setting is a reasonable cutoff.

- Ground-Glass Nodules (Figures 8, 9)
If the maximum diameter of a ground-glass nodule exceeds 15 mm on TS-CT, workup for definitive diagnosis is recommended, even if there is no change or if it increases on TS-CT after 3 months (Figure 8). If the maximum diameter is less than 15 mm, follow-up observation is conducted at intervals of 3, 12, 24, 36, 48, and 60 months on TS-CT (Figure 9): i) If there is an increase of 2 mm or more or an increase in attenuation, workup for definitive diagnosis is recommended. ii) If a solid component appears but its maximum diameter is less than 8 mm, further observation could be performed. iii) For GGNs that remain unchanged over five years of follow-up observation, it is recommended that follow-up at medical institutions for further investigations be terminated, but regular low-dose CT screening at the screening institution is recommended.

3. Points to Note in Reading, Pitfalls
In order to perform highly accurate lung cancer CT screening, we believe it is necessary to clarify the imaging characteristics of lung cancer that is easily overlooked and lung cancer that presents forms other than pulmonary nodules(Figure 10-12).The following are points to note when reading CT images.
- Even if the nodule diameter exceeds 10 mm, it may be overlooked.
- It is necessary to distinguish between pulmonary blood vessels and pulmonary nodules in areas such as near the hilum.
- Presence or absence of pulmonary nodules in contact with large blood vessels at the hilum or mediastinum (Figure 3).
- Presence or absence of lesions in the trachea or bronchi.
- Presence or absence of lesions in contact with the pleura (in addition to the peripheral subpleural lesions, interlobar pleura, mediastinum, and diaphragm), but differentiation from intrapulmonary lymph nodes in contact with the peripheral subpleural lesions or interlobar pleura is necessary (Figure 4, 5).
- Presence or absence of newly developed localized opacities in existing lesions (inflammatory scars or bullae in the apex of the lung, emphysema, interstitial pneumonia, etc.) (Figure 11). However, it may progress as a gradual increase in attenuation.
- Presence or absence of thickening of the walls of the lung cyst (Figure 2)
- Consideration of whether it can be judged as an "old lesion" (Figure 10)
- Presence or absence of lung nodules in other locations during the follow-up of the lung nodule detected at the initial examination
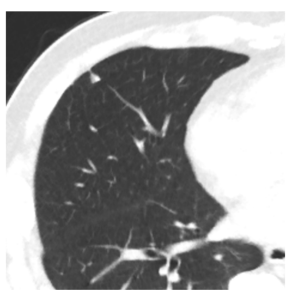
 Fig 10: Nodule Determined as Chronic Lesion Figure 10a The nodule in the left upper lobe was assessed as calcification due to the presence of chronic pulmonary tuberculosis in other areas. This assessment was performed during a CT scan conducted in the previous year, and no comparative reading was performed at that time. Figure 10b One year later, during a follow-up CT scan, the nodule in the left upper lobe was observed to have enlarged. Upon detailed examination, the nodule was diagnosed as small cell lung cancer with bone metastasis, stage IV. Comparative readings are necessary even for nodules classified as “chronic changes,” if previous CT images are available.
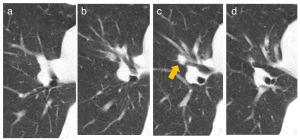
Fig 10: Nodule Determined as Chronic Lesion Figure 10a The nodule in the left upper lobe was assessed as calcification due to the presence of chronic pulmonary tuberculosis in other areas. This assessment was performed during a CT scan conducted in the previous year, and no comparative reading was performed at that time. Figure 10b One year later, during a follow-up CT scan, the nodule in the left upper lobe was observed to have enlarged. Upon detailed examination, the nodule was diagnosed as small cell lung cancer with bone metastasis, stage IV. Comparative readings are necessary even for nodules classified as “chronic changes,” if previous CT images are available. Fig 11: Band Opacity Appearing in Emphysema Figure 11a A screening CT image taken two years prior to referral to a medical institution. Moderate emphysematous changes are observed in the background lung, and a band opacity is noted near the pleura in right S3b. Figure 11b One year before the referral, the screening CT shows an increase in the attenuation value of the band opacity. Figure 11c At the time of referral to the medical institution, the width of the opacity in the dorsoventral direction had increased. Figure 11d a A thin-section CT image taken at the medical institution. Figure 11e Two months later, a follow-up thin-section CT image shows no temporal increase in the band opacity. Figure 11f Six months later, a significant increase in the proximal portion of the band opacity is observed. It was diagnosed as squamous cell carcinoma, cT2aN2M0. It should be noted that lung cancer does not always manifest as a typical pulmonary nodule morphology.
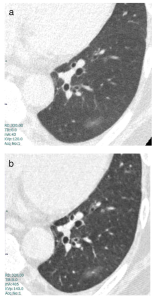
Fig 11: Band Opacity Appearing in Emphysema Figure 11a A screening CT image taken two years prior to referral to a medical institution. Moderate emphysematous changes are observed in the background lung, and a band opacity is noted near the pleura in right S3b. Figure 11b One year before the referral, the screening CT shows an increase in the attenuation value of the band opacity. Figure 11c At the time of referral to the medical institution, the width of the opacity in the dorsoventral direction had increased. Figure 11d a A thin-section CT image taken at the medical institution. Figure 11e Two months later, a follow-up thin-section CT image shows no temporal increase in the band opacity. Figure 11f Six months later, a significant increase in the proximal portion of the band opacity is observed. It was diagnosed as squamous cell carcinoma, cT2aN2M0. It should be noted that lung cancer does not always manifest as a typical pulmonary nodule morphology. Fig 12: Case with Temporal Enlargement of Mediastinal Lymph Nodes Figure 12a–12d Series of low-dose CT screening images 3 years prior, 2 years prior, 1 year prior, and at the time of diagnosis reveal the progression of findings. Figure 12a A round soft tissue nodule is noted adjacent to the intermediate bronchus (mediastinal lymph node #7) 3 years prior the time of diagnosis. Figure 12b, c The round soft tissue nodule showed mild enlargement two years prior to the diagnosis (b), followed by further enlargement one year prior (c). Figure 12d At the time of diagnosis, CT shows a large mass with 7cm in diameter, extending from the tracheal bifurcation to the surrounding vicinity of the opposite main bronchus. Ultrasound-guided bronchoscopic needle biopsy reveals the diagnosis of “mediastinal type” primary lung adenocarcinoma, cT0N3M0. Low-dose CT images should be interpreted with caution, as the image quality of soft tissues such as the mediastinum may degrade, posing challenges for evaluation. Even with low-dose imaging, ensuring image quality sufficient for evaluating soft tissues is desirable.
Fig 12: Case with Temporal Enlargement of Mediastinal Lymph Nodes Figure 12a–12d Series of low-dose CT screening images 3 years prior, 2 years prior, 1 year prior, and at the time of diagnosis reveal the progression of findings. Figure 12a A round soft tissue nodule is noted adjacent to the intermediate bronchus (mediastinal lymph node #7) 3 years prior the time of diagnosis. Figure 12b, c The round soft tissue nodule showed mild enlargement two years prior to the diagnosis (b), followed by further enlargement one year prior (c). Figure 12d At the time of diagnosis, CT shows a large mass with 7cm in diameter, extending from the tracheal bifurcation to the surrounding vicinity of the opposite main bronchus. Ultrasound-guided bronchoscopic needle biopsy reveals the diagnosis of “mediastinal type” primary lung adenocarcinoma, cT0N3M0. Low-dose CT images should be interpreted with caution, as the image quality of soft tissues such as the mediastinum may degrade, posing challenges for evaluation. Even with low-dose imaging, ensuring image quality sufficient for evaluating soft tissues is desirable.