RADIOLOGICAL REPORT
1. Review PREVIOUS STUDIES.
2. Description of the THYROID GLAND:
•DIMENSIONS of the two thyroid lobes (AP, T, and CC) and AP diameter of the isthmus.
•Description of the GLANDULAR PARENCHYMA (echogenicity, vascularization).
- Normal ECHOGENICITY is homogeneous and greater than neck muscles. In subacute/chronic thyroiditis we can find hypoechoic and poorly defined areas.
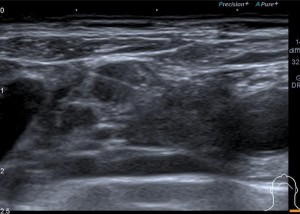
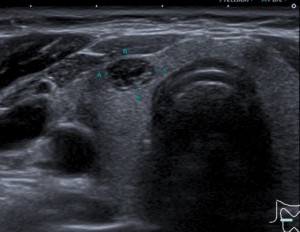
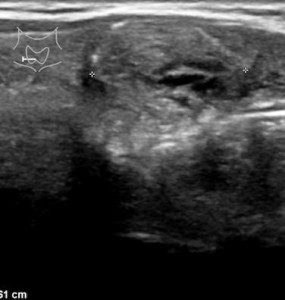
 Fig 1: Pseudonodular and hypoechoic area, and geographic borders measuring 6 x 12 mm, suggestive of an area of focal thyroiditis.
Fig 1: Pseudonodular and hypoechoic area, and geographic borders measuring 6 x 12 mm, suggestive of an area of focal thyroiditis. - VASCULARIZATION: can be altered in thyroiditis.
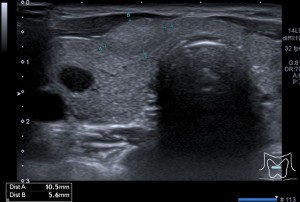
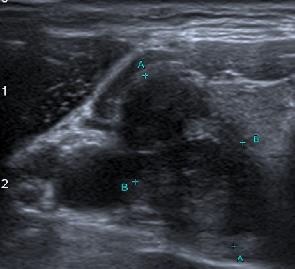
 Fig 2: The thyroid gland shows heterogeneity of its echostructure with increased vascularization, due to thyroiditis.
Fig 2: The thyroid gland shows heterogeneity of its echostructure with increased vascularization, due to thyroiditis.
3. Evaluate the LATEROCERVICAL lymph node CHAINS.
4. Description of the THYROID NODULES and other pathology
- Nodules smaller than 5mm should NOT be described. If greater than 5mm, images of the 3 dimensions should be taken in the sagittal and transverse planes.
- If there are multiple nodules, the radiologist should identify the 4 most suspicious nodules and describe them to facilitate follow-up in subsequent studies.
- Growth will be defined as: an increase in diameter of 20% or 2mm in two dimensions or an increase in volume of 50%
- If the TI-RADS category increases but does not meet the FNA criteria due to its dimensions, annual follow-up should be done.
IMAGING TECHNIQUES
ULTRASOUND
•Gold Standard.
•Its main role is to exclude nodules suspicious of thyroid cancer (7-15% of the detected nodules)
•It is performed with a high-frequency linear transducer (7Hz) and with the neck in hyperextension.
•LIMITATIONS:
•Inter-operator variability.
CEUS
Analyzes patterns of macro and microvascularization. Thanks to the incorporation of the latest generation contrasts, its applicability in thyroid pathology has increased. It detects malignant nodules with a sensitivity of 85% and a specificity of 82%.
•Classifications are currently being created, such as CEUS-TI-RADS. Some factors that are considered malignant according to CEUS-TI-RADS are:
- Centripetal/centrifugal enhancement
- Absence of ring enhancement
- Hypo-hyperenhancement
ELASTOGRAPHY
•Elastography in combination with B-mode ultrasound increases sensitivity and specificity in the characterization of thyroid nodules
•When compressed, pathological lesions are more rigid than the adjacent healthy tissue.
•LIMITATIONS:
•Those cancers with stroma similar to normal tissue, such as follicular cancer, will not be detected.
•It also does not give us information on nodules of a cystic nature or those with calcifications.
GAMMAGRAPHY
•It analyzes the uptake of a radioactive iodine marker (18F-FDG) by the thyroid. It is not recommended for the evaluation of previously diagnosed thyroid nodules, since thyroid uptake can be detected incidentally in up to 1-2% of patients.
•Uptake increases the risk of malignancy of the nodule, and clinical evaluation and FNA are recommended for nodules ≥1 cm that present high uptake.
•Nodules less than 1 cm, which do not meet the criteria for FNA, should be periodically reviewed by ultrasound.
ACR TI-RADS
The TI-RADS system was designed to reduce the number of biopsies of benign thyroid nodules and increase diagnostic accuracy. It evaluates 5 categories.
- COMPOSITION
- ECHOGENICITY
- SHAPE
- MARGINS
- PRESENCE OF CALCIFICATIONS
•A score is selected for each of these categories, according to the characteristics of the nodule.
•The total score obtained classifies the nodules into 5 types, from TI-RADS 1 (benign) to TI-RADS 5 (high suspicion of malignancy).
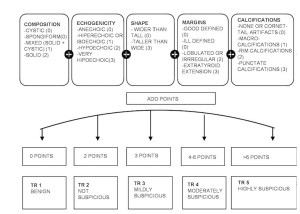
•From TI-RADS 3 onwards, FNA may be indicated.
EXAMPLES
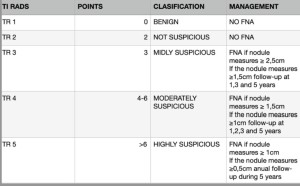
TI RADS 2
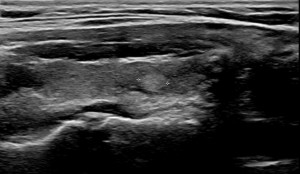
TI RADS 3

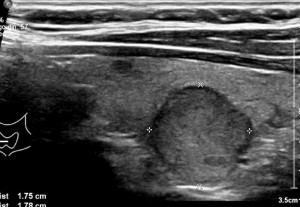
TI RADS 4

TI RADS 5


FNA
•It is the technique with more scientific evidence. It has a sensitivity of 65-98% and a specificity of 72-100% to detect thyroid cancer.
•LIMITATIONS:
It depends on the quality of the sample. It is indeterminate or non-diagnostic in 15-20% of patients. In these patients, the FNA is repeated; and if it remains indeterminate and malignancy is suspected, a thyroidectomy will be performed.
•Some characteristics related to non-diagnostic punctures are:
- macrocalcifications
- size <5-10mm
- cystic predominance
It should be limited to a MAXIMUM OF TWO suspicious NODULES (those with a greater TR) or any suspicious ADENOPATHY
•REQUIREMENTS:
- Coagulation between normal ranges.
- Informed consent.
- Material: gauze + chlorhexidine, 25 G or 22 G intramuscular needle, plastic syringe, slides.
- Posture: The patient will be placed in a supine position with a pillow underneath to facilitate hyperextension of the neck.
•PROCEDURE:
- Ultrasound will be performed to characterize the nodule and detect the adjacent vascularization, avoiding vascular structures.
- Prior asepsis with chlorhexidine.
- The needle must be parallel to the transducer leaving a separation of 1-2 cm to avoid contamination of the needle.
- Puncture of the thyroid nodule with aspiration and back-and-forth movement to obtain the maximum amount of material (for 5-10 seconds) trying to obtain a sample from the different quadrants of the nodule and the solid/suspicious areas, avoiding cystic areas and calcifications.
- Placement of the material on the slide.
•COMPLICATIONS: discomfort, hematoma, hemorrhage (due to puncture of vascular structures), vasovagal reaction…
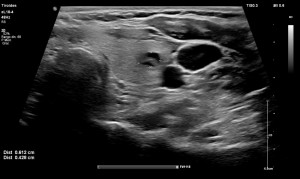
EXAMPLE OF AN FNA DONE ON A SUSPICIOUS ADENOPATHY