Findings and procedure details
Behçet’s disease affects arteries and veins of all sizes and types and is characterized by a variety of clinical manifestations due to its involvement with different types of vessels. Venular involvement and pulmonary arterial aneurysms are unique features of Behçet’s disease. Clinical manifestations can range from asymptomatic cases to life-threatening multi-organ involvement, leading to serious and potentially fatal complications such as cerebral vein thrombosis, intestinal perforation, occlusion of the VCI or VCS.
Thoracic manifestations
Behçet's disease can lead to aortic and pulmonary artery aneurysms, pulmonary infarction, and hemorrhage due to pulmonary thromboembolism. 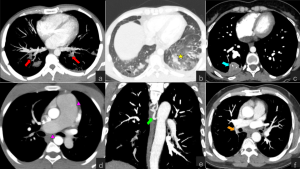
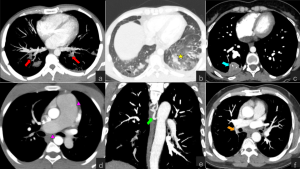
Fig 1: Involvement of pulmonary arteries and pulmonary thromboembolism in Behçet’s Disease. (a) Axial maximum-intensity-projection CTA of a 31 year-old male with Behçet’s disease presenting with dyspnea reveals thrombus in the subsegmental branches of bilateral pulmonary arteries (red arrows). (b-c) Axial CT images show ground-glass opacities in lower lobe of the left lung (asterisk) and wedge shaped peripheral opacity in the right middle lobe (blue arrow) as a result of pulmonary hemorrhage and infarction secondary to pulmonary embolism. (d) Axial CT image of a 45 year-old male with long standing Behçet’s disease shows enlargement of the pulmonary trunk and right pulmonary artery, suggesting pulmonary artery hypertension due to chronic pulmonary thromboembolism (pink arrowheads). (e) Coronal maximum-intensity-projection CTA of a 40 year-old female with Behçet’s disease, presenting with hemoptysis, reveals bronchial arterial enlargement (green arrow). (f) Axial Chest CTA image shows loss of calibration in the lower branch of the right pulmonary artery secondary to chronic pulmonary embolism (orange arrow).
Fig 2: Pulmonary artery aneurysms in Behçet’s Disease. (a-b) Axial and Coronal Chest CTA reveal multiple saccular aneurysms of proximal pulmonary arteries in a 18 year-old male with Behçet’s disease presenting with dyspnea (red arrows). (c) Axial CT image of a 37 year-old male with Behçet’s disease shows partially thrombosed left pulmonary artery (green arrow).
Cardiovascular manifestations
Vascular involvement is reported in approximately 50% of patients with Behçet's disease. The most common vascular manifestations include superficial vein thrombosis and deep vein thrombosis, predominantly in the lower extremities. More atypical sites can be affected, such as the inferior and superior vena cava, hepatic veins, and portal vein. Conditions like Budd-Chiari syndrome, Vena Cava Superior Syndrome or Vena Cava Inferior Syndrome can also occur. Fig 3: Venous involvement in Behçet’s Disease. (a) Coronal CT image of a 29 y/o male presenting with fever and severe abdominal pain shows a large occluding thrombus in inferior vena cava (red arrow). (b) Axial CT image of a 37 y/o female patient with Behçet’s Disease shows partial filling defect in left portal vein, compatible with thrombosis (green arrow). (c) In follow-up imaging of the same patient, axial CT image reveals cavernous transformation due to chronic occlusion of portal vein. (d-e) Axial and coronal CT images in venous phase of a 45 y/o male with Budd-Chiari Syndrome due to long-standing Behçet’s Disease show occlusion of the IVC and hepatic veins (asterisk), irregular liver borders (blue arrowheads), heterogeneous liver parenchyma and extensive retroperitoneal venous collaterals (orange arrowheads). Ascites and splenomegaly are also noted.
Fig 4: Venous involvement in Behçet’s Disease. (a-b) Coronal and axial Chest CTA of a 30 y/o female with long-standing Behçet’s demonstrate chronically occluded Vena cava superior (yellow arrows) and venous collaterals in mediastinum (red arrows). Bilateral pleural effusions are also noted. (c-d) Coronal and sagittal CT images of a 34 year-old male with Behçet’s Disease show Downhill esophageal varices secondary to SVC stenosis (blue arrows) and extensive venous collaterals in chest wall (green arrows).
Fig 5: Aortic involvement in Behçet’s Disease. (a) Axial CT image of a 34-year-old male patient with Behçet’s disease, presenting with chest pain, shows pseudoaneurysm of descending aorta with a surrounding soft tissue density (red arrowhead). Axial CT image following endovascular treatment of the same patient reveals TEVAR stent-graft for aortic aneurysm and endoleak (asterisk). (c-d) Axial and Coronal CTA of a 42 y/o female patient with Behçet’s disease, presenting with sudden-onset abdominal pain, reveal a large ruptured abdominal aortic aneurysm (orange arrowheads). (e) Axial CT image following endovascular treatment of the same patient reveals uncomplicated EVAR stent (green arrowhead) and retroperitoneal hematoma (pink arrowhead), there is no contrast extravasation.
Fig 6: Arterial involvement in Behçet’s Disease. (a) Coronal maximum-intensity-projection CT image of a 51 y/o female patient with Behçet’s disease presenting with abdominal pain, shows extensive aortitis involving the infrarenal aorta and left common iliac artery, with a soft tissue density surrounding it, leading to mural irregularity and luminal narrowing (red arrows), focal stenosis in the left renal artery (red arrow), suprarenal abdominal aortic pseudoaneurysm (orange arrow) and occluded right common iliac artery (asterisk). (b) Sagittal CT image of the same patient reveals mural irregularity, luminal narrowing in superior mesenteric artery and celiac artery (green arrowhead).
Fig 7: Pseudoaneurysm of peripheral arteries in Behçet’s Disease. (a-b) Color Doppler Ultrasound shows swirling flow within the pseudoaneurysm at the lower segment of the left superficial femoral artery, with a narrow neck in an 18 y/o male with Behçet’s disease. (c-d) Coronal CTA images reconstructed with maximum intensity projection confirm large pseudoaneurysm of the left superficial femoral artery (arrows).
Gastrointestinal manifestations
Gastrointestinal involvement in Behçet's disease often manifests as mucosal ulcerations, primarily in the terminal ileum, cecum, colon, and esophagus. Imaging studies may reveal mucosal irregularity, asymmetric wall thickening, and mucosal enhancement in areas affected by the disease. Extensive ulcerations, particularly in the ileocecal region, can lead to intestinal perforation or hemorrhage. Fig 8: Gastrointestinal involvement in Behçet’s Disease. (a-b) Axial and coronal CT images of a 30-y/o male patient presenting with abdominal pain who previously underwent ileocecal resection of terminal ileum due to Behçet's disease, show diffuse wall thickening and mucosal enhancement in the distal ileum (red arrows), along with intraperitoneal free air suggesting intestinal perforation (blue arrow). (c) Coronal CTA of the same patient reveals irregular wall thickening and mucosal enhancement in the duodenum (orange arrow). (d) Axial CT image of a 41-y/o male patient similarly shows irregular wall thickening due to involvement of Behçet's disease (green arrowhead).
Musculoskeletal Manifestations
Inflammatory, non-erosive arthritis is observed in approximately 50% of patients with Behçet's disease. Joint involvement is primarily peripheral, with the knees being the most commonly affected joints; spine involvement or sacroiliitis is rare. Fig 9: Musculoskeletal involvement of Behçet’s Disease in a 39 year-old female presenting with hip pain. (a) Coronal STIR image shows high signal intensity at the sacral sides of sacroiliac joints, suggesting bone marrow edema (red arrows). (b) T1W axial image reveals low signal intensity and irregularity of joint surfaces suggesting erosions and sclerosis in both sacroiliac joints (yellow arrows). Post-contrast T1W axial image demonstrates contrast enhancement at the same area compatible with active inflam
Fig 10: Musculoskeletal involvement of Behçet’s Disease in a 22 y/o female patient presenting with right knee pain. (a-b) Coronal and axial STIR images of proximal cruris show increased signal intensity in muscle planes suggesting edema and inflammation (red arrows). (c-d) Pre/Post-contrast T1W axial images demonstrate enhancement in the muscle planes compatible with myositis (orange arrow). (e) Sagittal PDW fat-sat image of right knee shows effusion and increased signal intensity in the synovium of the knee joint (green arrows) and (f-g-h) pre/post-contrast T1W axial and sagittal images demonstrate synovial thickening and enhancement extending into muscle planes, indicating synovitis of the knee joint (blue arrows). After steroid treatment, the patient's clinical findings improved significantly. Myositis is an uncommon manifestation in Behçet’s disease.
Neurological Manifestations
Neuro-Behçet’s disease affects around 5% of patients. There are two major categories of CNS involvement: parenchymal and less often non-parenchymal. Parenchymal involvement characteristically involves the upper brainstem. Other sites of parenchymal involvement are the subcortical white matter, thalamus, basal ganglia and the spinal cord. In Neuro-Behçet's disease, MRI findings in affected brain regions often show increased T2W/ FLAIR signals reflecting vasogenic edema during the active phases of the disease, along with contrast enhancement in active lesions.In chronic cases, affected regions may display gliotic changes and atrophy. Since MRI findings are not specific to neuro-Behçet's disease, imaging features should always be evaluated with the patient's medical history and clinical manifestations.
Fig 11: Involvement of Brain Parenchyma in Neuro-Behçet’s. (a-b-c-d) FLAIR image (a) shows a focal area of higher signal intensity on the left side of pons in a 42 y/o female with Behçet’s Disease presenting with acute visual disturbance (yellow arrow). Post-contrast T1W axial image (b) shows slight peripheral enhancement around the lesion (green arrow). DWI-ADC images (c-d) show restricted diffusion (red arrows). (e-f) T2/FLAIR images show a focal area of higher signal intensity in right cerebral peduncle in a 39 year old male with Behçet’s Disease presenting with postural instability and dysarthria (red arrowheads). After immunosuppressive therapy,previous pathologic signal changes are regressed (g-h) (yellow arrowheads) indicating response to treatment. Upper brainstem involvement is characteristic for Neuro-Behçet’s disease.
Fig 12: Neuro-Behçet Parenchymal Involvement. (a-b-c-d) Abnormal T2W/FLAIR hyperintense (a-b), T1W hypointense (c) signal changes affecting the right basal ganglia are noted in a 39 y/o male patient with Behçet’s Disease presenting with postural instability and dysarthria (red arrowheads). Post-contrast T1W axial image (d) shows slight patchy enhancement in right basal ganglia (green arrowhead). After immunosuppressive therapy, there are no abnormal signals or enhancement in the right basal ganglia on T2W/FLAIR (e,f) and Pre/Post-contrast T1W images (g,h), indicating improvement of inflammation (white arrowheads).
Fig 13: Neuro-Behçet’s Non-Parenchymal Involvement. (a-b-c-d) A 15 y/o male with a history of Behçet’s disease presents with headache. Coronal post-contrast T1W (a) and MIP images (b) show a filling defect (red arrows) due to acute thrombus in left transverse sinus. A year after treatment MR-V MIP images (c) show irregularly narrowed left transverse sinus with recanalized flow (blue arrowheads). Post-contrast T1W axial image (d) shows venous collaterals around the midbrain (green arrows).