I.Mechanisms of injury according to the TLICS:
The TLICS classification system provides a spine injury severity score that is based on 3 items: injury morphology, integrity of the posterior ligamentous complex (PLC) and neurologic status of the patient.
The total assigned TLICS score represents a prognostic value and guide the indication of surgical management. This classification system focuses on the importance of stable vs instable injuries, instable injuries being those with implication of the PLC and where spine injuries are more frequent, and thus emphases on the important role of MRI. It also acknowledges that the patient’s neurological status is the main driver of surgical intervention.

A) Injury Morphology :
TLICS identifies three mechanisms of fractures: compression, translation/rotation, and distraction fractures.

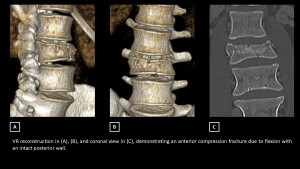
Compression injuries are characterized by a loss of vertebral height or disruption of the vertebral endplate. Less severe cases affect only the anterior portion of the vertebra, while more severe cases result in burst fractures involving the posterior vertebral body. These may include retropulsion or the presence of osseous fragments in the spinal canal, potentially leading to spinal cord compression. These injuries are primarily caused by axial loading.
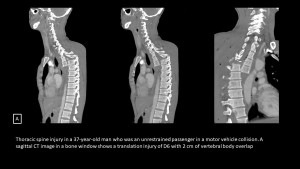
Translation injuries involve the horizontal displacement or rotation of one vertebral body relative to another. These injuries result from torsional or shear forces and are marked by the rotation of spinous processes, unilateral or bilateral facet fracture-dislocations, and vertebral subluxations.


Distraction injuries are identified on imaging by anatomic separation along the vertical axis. They may occur through the anterior and posterior supporting ligaments, the osseous elements, or a combination of both. A Chance fracture, also known as “seatbelt fracture”, is a flexion-distraction injury involving all three spinal columns (anterior, middle, and posterior). It is commonly associated with intra-abdominal injuries, particularly affecting the pancreas, duodenum, and traumatic arterial dissections, with the superior mesenteric artery being most frequently involved.

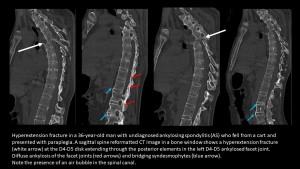
Distraction fractures in hyperextension are the most frequently observed in patients with a rigid spine. The fracture line may be trans osseous, osseous and ligamentous, or trans discal. In cases of ankylosing spondylitis, the fracture line is often trans discal. These fractures are highly unstable and are commonly accompanied by neurological complications with the rates of such complications ranging from 33% to 58% in thoracic and lumbar regions [2,3].
When multiple injury morphologies are present, the injury with the highest score is used for classification. In cases where injuries involve multiple levels, each injury is evaluated individually.
B) PLC status:
PLC plays a vital role in maintaining spinal stability. It comprises the supraspinous ligament, interspinous ligament, facet capsules, and ligamentum flavum, collectively functioning as the spine's posterior tension band.
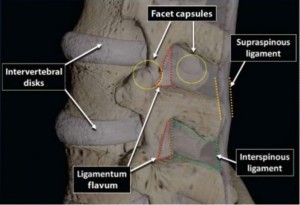
The PLC protects the spinal column from excessive flexion, rotation, translation, and distraction forces. The TLICS places significant emphasis on assessing PLC integrity, as these structures have limited healing potential and typically require surgical intervention when disrupted. Disruption of PLC is suggested on CT scans by findings such as widening of the interspinous space, avulsion fractures at the superior or inferior edges of adjacent spinous processes, widening, perched or dislocated facet joints, and vertebral body translation or rotation.
C) Neurological status :
The patient's neurologic status is a crucial factor in assessing the severity of spinal column injuries. The TLICS system assigns scores based on neurologic status, with 0 points for intact function, 2 points for nerve root or complete spinal cord injury, and 3 points for incomplete spinal cord injury or cauda equina syndrome. The higher score for incomplete injuries reflects a greater potential for surgical benefit.
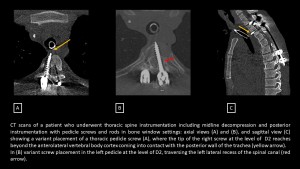
It is also important to highlight that the CT scan plays a vital role in postoperative evaluation, especially in confirming the fracture reduction and ensuring the correct positioning of the orthopedic fixation devices.
II. Role of MRI :
Even though CT scans can predict the rupture of the posterior ligamentous complex, MRI remains the gold standard for its assessment [4].
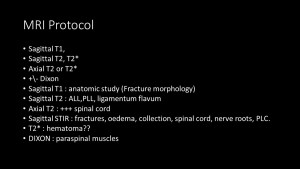
The MRI protocol includes sagittal T1, T2, T2*, and STIR sequences, along with axial T2/T2* sequences. The gradient echo sequence plays a critical role in detecting susceptibility effects, which are indicative of cord hemorrhage or hematoma.
The ligamentum flavum and the supraspinous ligament are evaluated on sagittal T1, T2, sequences as low-signal-intensity continuous black stripes. The interspinous ligament is visualized on STIR sequences. The involvement of the capsuloligamentous structures of the posterior facets is assessed on axial T2/FS sequences. A complete ligament rupture is indicated by a hypersignal on T2-weighted images with disruption of ligamentous continuity whereas STIR an edematous signal with no visible structural changes are indicative of partial tears or ligament strains and considered as indeterminate finding according to the TLICS and thus given a score of 2.
A) Acute cord injury :
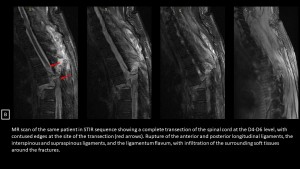
Traumatic spinal cord injuries vary and range from a spinal cord concussion, which is invisible on imaging, to complete spinal cord transection [5]. Spinal cord edema appears as a high T2 signal and a normal or low T1 signal within the cord. Hemorrhagic cord contusion appears as a central intramedullary focus of low signal T2* within the cord, surrounded by a thick rim of hyperintensity on T2W or T2*W GRE imaging, indicating edema. If the lesion exceeds 4mm in size, it is classified as a cord hematoma. In contrast, edematous contusion shows only the intramedullary hypersignal on T2 [5]. Cord transection is the most severe type of spinal cord injury, characterized by a complete disruption of the cord. High-signal cerebrospinal fluid is visible between the severed ends of the cord on T2W images.
B) ligamentous injury :
Spinal ligaments typically appear as low signal intensity bands on imaging. Ligamentous tears can be partial, showing high signal areas on STIR images due to edema and hemorrhage, with some intact fibers, or complete, where there is a total loss of intact fibers and high signal intensity from associated edema and hemorrhage [6].
C) Extra medullary hemorrhage and fluid collections:
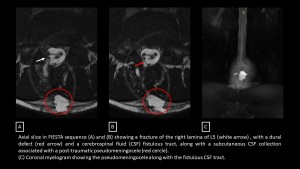
Extradural hematoma is the most common type of extra-medullary collection in trauma patients. Subdural hematoma and subarachnoid hemorrhage are less common. Other rare complications of spinal trauma include pseudomeningoceles and extradural fluid collections resulting from dural tears.
D) Vascular injuries:
In thoracolumbar spine trauma, injuries to the aorta and its branches can occur, particularly in cases of Chance fractures. Imaging findings of vascular injuries include the presence of an intimal flap, pseudoaneurysm, dissection with intramural hematoma, complete occlusion, and active extravasation.