The knee joint is a hinge joint (at least two bones with articular surfaces covered by hyaline cartilage and lubricated by synovial fluid) between the femur, tibia, and patella. [1]
Knowledge of basic knee anatomy is crucial for accurate and complete radiological diagnosis. Figure 1 illustrates a few of the anatomical landmarks commonly seen affected on knee MRIs.

MRI PROTOCOL AND SEQUENCES (Figure 2)
Knee MRI protocols typically include axial, coronal, and sagittal imaging with fluid-sensitive sequences. [2]
T1-weighted images evaluate soft tissues and tissues that contain more fat.
- tissues that predominantly contain fat (bone marrow) - high T1 signal
- tissues that contain more water (ligaments, cartilage, synovial fluid) - low T1 signal [3]
T2-weighted images evaluate tissues that contain more water.
- tissues such as ligaments, cartilage and fluids - high T2 signal
- bone marrow - high T2 signal [3]
Proton density (PD) images minimize the contribution of both T1 and T2 and have better contrast by enhancing structures with a higher proton density.
- fatty bone marrows and hyaline cartilage - high PD signal
- muscles - intermediate PD signal
- ligaments - low PD signal [3]
Intravenous contrast is useful for evaluating synovitis, tumours, and infection, and can be used to obtain an indirect arthrogram. [2]

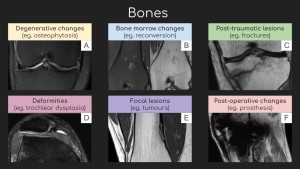
BONES (Figure 3)
Common pathologies affecting the knee joint bones (distal femur, proximal tibia, fibular head, and patella) include:
Degenerative changes [4]
- altered shape of the tibial plateau and femoral condyles
- subchondral sclerosis
- subchondral bone marrow oedema and cysts (geodes)
- marginal osteophytes
Deformities and anatomical variants [5, 6]
- trochlear dysplasia
- a shallow, flattened or convex trochlear groove and a hypoplastic or convex lateral femoral condyle (a sulcus angle of >145-150 degrees)
- associated with patellofemoral instability and recurrent patellar dislocation
- bipartite patella (kneecap divided into two separate bones)
- sesamoid bones: fabella (in the lateral head of the gastrocnemius tendon)
Bone marrow changes [6]
- red marrow: low T1 and high T2 signal, high FS signal
- yellow marrow: high T1 and T2 signal, low FS signal
- marrow reconversion (in increased hematopoietic demand): red marrow signal
- marrow oedema: intermediate T1 signal, high T2 FS signal
Focal lesions [7]
- chondrogenic tumours (eg. osteochondroma)
- osteogenic tumours (eg. osteoma, osteosarcoma)
- fibrogenic tumours (eg. fibroma, fibrosarcoma)
- vascular tumours (eg. hemangioma, angiosarcoma)
- osteoclastic giant cell-rich tumours (eg. aneurysmal bone cyst, non-ossifying fibroma)
- metastases
Post-traumatic lesions
- fractures
- dislocations
- bone marrow oedema
Post-operative changes
- metallic knee arthroplasty implants
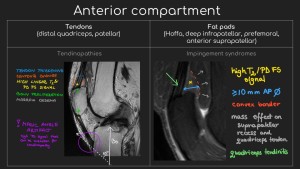
ANTERIOR COMPARTMENT (Figure 4)
The structures most commonly affected in the anterior compartment of the knee are:
Tendons (distal quadriceps, patellar) [2, 8]
- traumatic injury (partial tear, rupture) - linear interfibrillar high T2 signal intensities
- tendinopathy (reactive, tendon disrepair, degenerative)
- false positive tendinopathy - magic angle artefact (collagen fibres are oriented 55 degrees relative to the magnetic field)
- patellar height
- Insall-Salvati ratio (ISR) - the ratio of the patella tendon length to the length of the patella
- patella alta (high patella) - ISR > 1.5
- patella baja (low patella) - ISR < 0.8
Fat pads [6]
- impingement syndromes
- anterior suprapatellar fat pad (quadriceps)
- infrapatellar fat pad (Hoffa) - repetitive traumas, patella alta
- femoral fat pad impingement syndrome - osteophytosis, patellar tendon-lateral femoral condyle friction syndrome
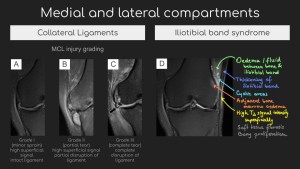
MEDIAL AND LATERAL COMPARTMENTS (Figure 5)
Collateral ligaments - stabilisation of side-to-side movements [2, 9]
- MCL (medial collateral ligament) - prevention of inward movement
- LCL (lateral collateral ligament) - prevention of outward movement
Iliotibial band syndrome [2, 9]
- chronic inflammation of the fat adjacent to the iliotibial band
- associated with limb length discrepancy, genu varum, overpronation
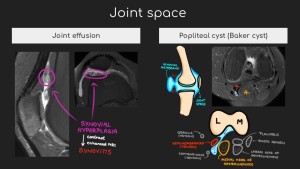
JOINT SPACE (Figure 6)
Joint effusion [2, 10]
- physiological small amount of intra-articular fluid
- causes: trauma, inflammation, infection
- loose bodies (post-traumatic, osteoarthritis)
- lipo-hemarthrosis (fat-fluid level) - in cases of intraarticular fractures due to marrow fat leakage
- synovitis - synovial hyperplasia and enhancement on post-contrast imaging
Cysts [2]
- ganglion cysts - lined by fibrous connective tissue
- synovial cysts - lined by synovium
- posterior knee - popliteal cyst (Baker’s cysts) - between the medial head of the gastrocnemius muscle and the semimembranosus tendon
- complications: haemorrhage, leakage, rupture
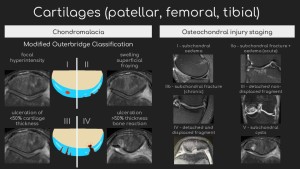
CARTILAGES (Figure 7)
Chondral lesions [11]
- usually progress slowly and clinical manifestations appear with time
- high PD and T2 signal
- chondral tapering
- loss of definition of the cartilage margins
- surface irregularities
- most frequent locations: medial femoral condyle, lateral tibial plateau
Osteochondral injury [11]
- focal areas of cartilage injury and damage to the adjacent subchondral bone plate and subchondral cancellous bone
- rim sign (high signal line) outlining bone fragment - unstable lesion
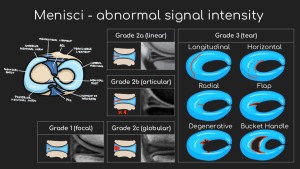
MENISCI (Figure 8)
Tears [12]
- meniscal distortion in the absence of prior surgery
- increased signal intensity in contact with the articular surface
- “two-slice-touch” rule - findings can be seen on at least two consecutive images in the same plane or at least two planes
- increased intradiscal high signal is often not associated with a tear intraoperatively
- indirect signs of meniscus tear
- parameniscal cysts (in contact with the torn meniscus)
- meniscus extrusion (>3 mm extension of the meniscus beyond the tibial plateau)
- subchondral marrow oedema (superficial, adjacent to the meniscus attachment, parallel to the articular surface, <5 mm deep)
Anatomic variants [12]
- discoid meniscus - enlarged meniscus with central extension onto the tibial plateau
- meniscal flounce - “wavy” appearance of the non-anchored inner edge of the meniscus
- meniscal ossicle
- chondrocalcinosis - increased diffuse intradiscal signal intensity
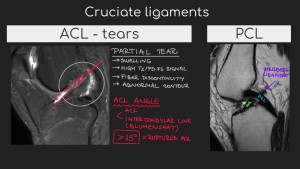
CRUCIATE LIGAMENTS (Figure 9)
Cruciate ligament tears [6]
- ACL (anterior cruciate ligament)
- ligament swelling, discontinuity, non-visualization, or mass replacement (oedema, haemorrhage)
- ACL angle (between intercondylar Blumensaat line and ACL) >15 degrees - ACL rupture
- empty notch sign (avulsion of the femoral attachment)
- scarring of torn ACL to the PCL, roof of the intercondylar notch, or lateral femoral condyle
- bone contusion (lateral femoral condyle, lateral tibial plateau)
- anterior tibial translation
- positive PCL line sign
- Segond fracture (avulsion fracture of the lateral tibial plateau)
- PCL (posterior cruciate ligament)
- anterior meniscofemoral ligament (ligament of Humphrey)
- posterior meniscofemoral ligament (ligament of Wrisberg)
- usually remains contiguous
- absent PCL - high T1 and T2 signal
- ligament swelling (>7 mm)
- posterior tibial translation
- false positive PCL tear - variant anatomy
Mucoid degeneration
- thickening with a “celery stalk” appearance
- can mimic acute or chronic interstitial partial tears
Ligament grafts
- complications: impingement, rupture, rejection
SOFT TISSUES
Bursitis
- prepatellar
- infrapatellar - superficial or deep to the distal insertion of the patellar tendon
Muscular pathologies [13]
- atrophy (fatty infiltration)
- muscle injury
- musculotendinous injury
- chronic disuse
- denervation
- myopathy (eg. muscular dystrophy)
- corticosteroid use
- oedema (low T1 signal and high T2 signal)
- traumatic injury
- muscular exertion
- rhabdomyolysis
- vascular insults (eg. compartment syndrome)
- myositis (eg. autoimmune, infectious, early myositis ossificans)
- focal lesions
- infection (eg. abscess)
- trauma (eg. haematoma)
- myonecrosis
- neoplasms (eg. lipoma, leiomyosarcoma)
Vascular pathology [14]
- anatomy variants
- trauma
- posterior knee dislocations - traumatic dissection of the popliteal artery or vein
- anterior knee dislocations - intimal tractions and tears
- popliteal artery entrapment syndrome - under the medial head of the gastrocnemius muscle
- popliteal vein thrombosis
- soft tissue oedema around the vessel
- vein distension
- venous collaterals
- contrast-enhanced images - filling defect, intraluminal web
- arterial atherosclerotic stenoses
- popliteal artery aneurysms
- atherosclerotic disease, trauma, Behcet disease, Marfan syndrome
- complications: rupture, thrombosis (multiple concentric rings of signal abnormality), distal embolisation - risk of acute leg ischemia
- cystic adventitial disease -nonatherosclerotic benign lesion
- vascular malformations