Certain cholecystitis complications are interrelated, with some serving as intermediate steps to others.
These may mimic malignancy on imaging, complicating preoperative diagnosis. Gallbladder tumors are often misdiagnosed due to overlapping clinical and imaging features with benign entities, requiring a holist approach that integrates clinical, pathological and radiological expertise.
Gallbladder wall thickening has limitations as a diagnostic marker for acute cholecystitis, presenting a wide differential diagnosis, including:
-Cholecystitis;
-Postprandial pseudothickening;
-Secondary thickening (e.g., hepatic cirrhosis, congestive right heart failure, ascites and other acute inflammatory processes in the right upper quadrant);
-Gallbladder carcinoma;
-Diffuse adenomyomatosis;
-Etc.
ACUTE UNCOMPLICATED CHOLECYSTITIS
Acute cholecystitis develops in 90% of cases due to lithiasis, following a sequence of events that begins with gallstone obstruction, followed by inflammation, increased intraluminal pressure, impaired venous and lymphatic drainage, vascular compromise, necrosis and perforation.
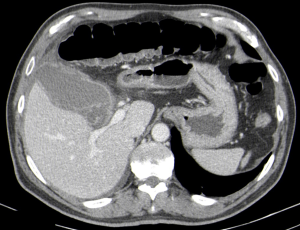
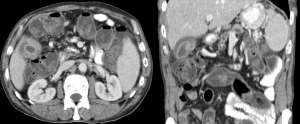
CT findings:
-Gallbladder distension and wall thickening (>3 mm);
-Regular mucosal or mural enhancement;
-Perivesicular fluid;
-Inflammatory fat stranding;
-Cholelithiasis/increased bile density;
-Transitory enhancement of the adjacent liver suggesting reactive hyperemia and inflammation.
Gallstones can appear as hyperdense (calcified), soft tissue or fat density, isodense with bile (possibly missed on CT, mimicking acalculous cholecystitis), gas-containing, etc.
Acalculous cholecystitis often affects critically ill patients (trauma, major surgery, sepsis, total parenteral nutrition, etc). These conditions can promote bile stasis, inflammation and reduce gallbladder perfusion. Diagnosis is frequently delayed because comorbidities lessen the accuracy of clinical and imaging findings, requiring heightened suspicion.

COMPLICATED ACUTE CHOLECYSTITIS
GANGRENOUS CHOLECYSTITIS
The most common complication of acute cholecystitis, usually due to severe and prolonged inflammation, where increased intraluminal pressure impairs wall vascularization, causing ischemia and necrosis. Risk factors include age, male sex, delayed surgery, diabetes and cardiovascular disease. Murphy’s sign may be absent due to ischemic denervation.
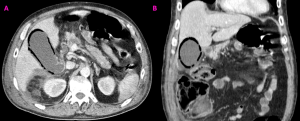
CT findings:
-Acute cholecystitis features;
-Irregular wall thickening;
-Focal wall irregularity or defect;
-Intraluminal membranes;
-Absence of mural enhancement (focal or diffuse).
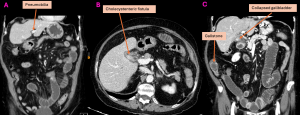
EMPHYSEMATOUS CHOLECYSTITIS
Rare acute cholecystitis variant that primarily affects elderly men with diabetes. It’s secondary to ischemia of the gallbladder wall and subsequent proliferation of gas-forming bacteria.
CT findings:
-Air in the gallbladder lumen or wall;
-No cholecysto-enteric fistula;
-Pneumoperitoneum suggests perforation.
HEMORRHAGIC CHOLECYSTITIS
Inflammatory process of the gallbladder complicated by hemorrhage into the lumen. The cause is unclear but may involve mucosal necrosis with bleeding from small wall vessels, cystic artery pseudoaneurysm rupture, etc. Clinically, it mimics acute cholecystitis, but may also present with hematemesis, melena and obstructive jaundice from bile duct clots.
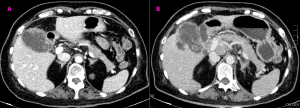
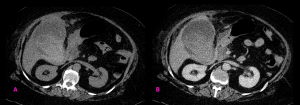
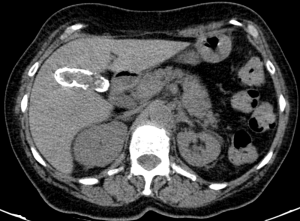
Ct findings:
-Acute cholecystitis features;
-High-density material within the lumen; it may appear swirling or layering, depending on the time between onset and imaging;
-Free intraperitoneal fluid, indicating possible perforation;
-Search for active contrast extravasation;
Distinction must be made between biliary sludge, layering gallstones, milk of calcium or vicarious excretion from prior intravenous contrast administration.
PERFORATED CHOLECYSTITIS
Serious complication of an advanced stage of acute cholecystitis, which may complicate emphysematous, gangrenous or hemorrhagic cholecystitis.
CT findings:
-Acute cholecystitis features;
-Discontinuity of the gallbladder wall;
-Extraluminal gallstone;
-Free intraperitoneal gas/fluid/blood;
-Pericholecystic fluid collection;
-Fistula formation;
-Gallbladder lumen collapse.
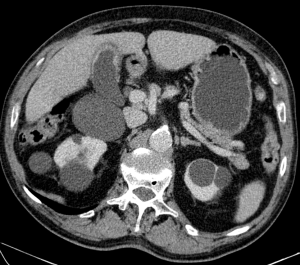
GALLBLADDER EMPYEMA
Uncommon complication of cholecystitis characterized by a gallbladder lumen filled and distended with purulent material, unable to drain due to an obstructive stone/mass.
CT findings:
-Acute cholecystitis features;
-High-attenuating material in the lumen (nonspecific).
VASCULAR COMPLICATIONS
VISCERAL ARTERIES PSEUDOANEURYSM
Severe gallbladder inflammation can erode and weaken the adjacent arterial wall (usually cystic or right hepatic arteries), leading to pseudoaneurysm formation. It’s often an incidental finding but can cause haemobilia, upper GI hemorrhage or hemoperitoneum if ruptured.
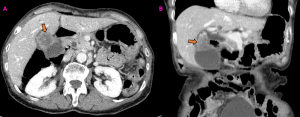
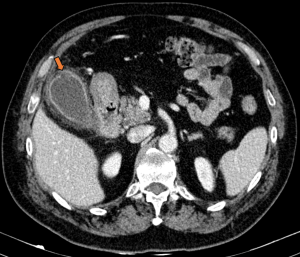
CT findings:
-Pericholecystic inflammation;
-Abnormal vessel dilation, usually eccentric, with attenuation similar to the artery/aorta;
+/- Spontaneous hyperattenuating intraluminal hemorrhage (if ruptured);
+/- Surrounding hematoma (if ruptured);
+/- High-density material in biliary ducts (if hemobilia).
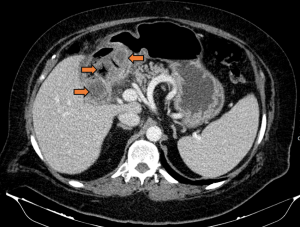
SEPTIC PYLEPHLEBITIS
Thrombotic occlusion of the portal vein and its branches, secondary to a proinflammatory state associated with infections in regions draining into the portal venous system, such as cholecystitis.
CT findings:
-Enlarged portal vein with lack of enhancement;
-Hepatic artery overflow may cause transient enhancement of adjacent liver parenchyma during the arterial phase;
-Complications: bowel ischemia, intra-abdominal abscesses, etc.
OTHERS
CHRONIC CHOLECYSTITIS
Chronic gallbladder inflammation, almost always due to cholelithiasis, may be asymptomatic or present with recurrent acute cholecystitis or biliary colic. Imaging may reveal cholelithiasis, wall thickening with either gallbladder contraction or distension. Pericholecystic inflammation is typically absent. Correlating imaging findings with clinical presentation is essential.

GALLBADDER VOLVULUS
A rare cause of acute abdomen, characterized by gallbladder rotation around the cystic duct and artery, potentially causing vascular compromise and gallbladder ischemia. It may lead to superimposed acute cholecystitis.
CT findings:
-Gallbladder displaced from its normal fossa;
-Change in gallbladder anatomical orientation;
-Gallbladder distension;
-Cystic duct abrupt tapering;
-“Swirl sign” of vascular pedicle;
-Pericholecystic fluid;
-Loss of wall enhancement.
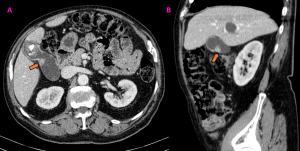
MIRIZZI SYNDROME
Extrinsic compression of an extrahepatic biliary duct by a stone in the cystic duct or gallbladder neck. It can mimic other pathologies like cholangiocarcinoma. Prolonged obstruction may lead to superimposed acute cholecystitis and fistula formation.
CT findings:
-Impacted stone in gallbladder neck/cystic duct;
-Dilated extrahepatic ducts gradually tapering to a normal common bile duct;
-Acute cholecystitis features.
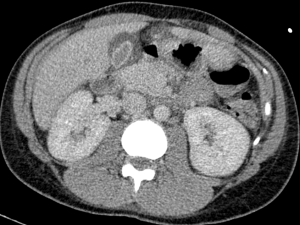
XANTHOGRANULOMATOUS CHOLECYSTITIS
A rare variant of chronic cholecystitis, characterized by focal or diffuse transmural histiocyte infiltration. It´s believed to result from rupture of occluded Rokitansky-Aschoff sinuses, leading to bile extravasation in the wall and a xanthogranulomatous inflammatory reaction. This leads to the formation of multiple wall nodules corresponding to foamy cell infiltration or abscesses.
CT findings:
-Focal/diffuse asymmetric wall thickening;
-Hypodense intramural nodules;
-Mucosal continuity maintained;
-Features of local infiltration (the extensive inflammation may involve adjacent organs, mimicking neoplasm) and other complications (e.g., abscesses).
PORCELAIN GALLBLADDER
Complete or partial calcification of the gallbladder wall. The incidence of gallbladder carcinoma is not significantly higher than in the general population; however, due to its high mortality, prophylactic laparoscopic cholecystectomy remains recommended.
CT findings:
-Thin mineralization layer outlining the gallbladder wall.
GALLSTONE ILEUS
Rare complication of chronic cholecystitis in which a gallstone passes through an enterobiliary fistula, becoming impacted typically at the ileocecal valve, causing small bowel obstruction. It’s characterized by Rigler’s triad: pneumobilia, small bowel obstruction and an ectopic calcified gallstone.
BOUVERET SYNDROME
Gastric outlet obstruction secondary to impaction of a gallstone in the pylorus or proximal duodenum.
ADENOMYOMATOSIS
It’s one of the hyperplastic cholecystosis of the gallbladder wall. Three morphological types are described: fundal/localized, segmental (annular) and generalized. CT features include focal or diffuse gallbladder wall thickening and observation of intramural diverticula (small, round, intramural hypodense lesions).
Differentiating from malignancy can be challenging. Some authors consider that a two-layer pattern suggests malignancy if the enhancing inner layer is thicker than the hypodense outer layer; or if a single thick enhancing layer is present. Wall calcifications in the thickened segment may also favor malignancy.
GALLBLADDER TUMORS
These tumors are often detected at an advanced unresectable stage due to their typically asymptomatic nature. They share clinical and imaging features with benign conditions, particularly in the early stages, complicating the differential diagnosis. The challenge increases when carcinoma coexists with benign conditions.
CT findings:
-Intraluminal polypoid mass (15-25%): A size exceeding 1 cm (the main malignancy predictor), sessile morphology, focal wall thickening or basal wall indentation favor malignancy. Conversely, multiple masses favor benignity.
-Diffuse or focal mural thickening (20-30%): usually asymmetric, irregular or nodular, and often exceeding 1 cm in thickness. it may exhibit marked arterial phase enhancement that persists or becomes isodense to the liver in the portal venous phase. Features suggesting neoplasm include loss of the gallbladder-liver interface, wall calcifications, biliary obstruction, adenopathy and metastases.
-Mass replacing the gallbladder (40-65%): This likely represents progression from previous patterns. It can potentially directly invade the surrounding liver parenchyma. It may exhibit necrotic areas or trapped bile and can present with calcifications linked to engulfed gallstones, porcelain gallbladder or tumor calcifications. Gallbladder cancer is typically hypodense and heterogeneous on unenhanced CT, with about 40% displaying hypervascular foci after IV contrast. Large lesions may show intense and irregular peripheral enhancement during the early arterial phase. Additionally, contrast enhancement may persist in fibrous stromal components of gallbladder carcinoma during portal venous and delayed phases (distinguishing it from the washout pattern of hepatocellular carcinomas).