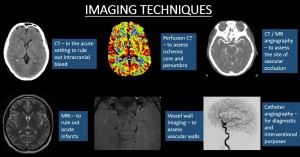
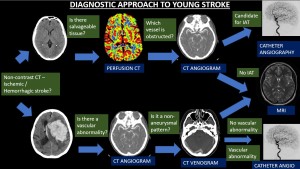
ROLE OF IMAGING
1. Non-contrast CT and MRI
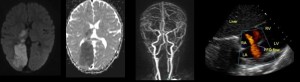
In the acute setting, CT is the most preferred investigation modality due to its speed and wide availability, which allows faster assessment to rule out intracranial hemorrhage and to initiate treatment with tPA in appropriate patients. Acute stroke evaluation with MRI is gaining popularity owing to its increased sensitivity and decreasing imaging times. Stroke MRI protocols with non-enhanced Diffusion weighted imaging (DWI), gradient-echo imaging, and fluid-attenuated inversion-recovery (FLAIR) imaging along with time of flight (TOF) non-contrast MR angiography of the head and neck can be performed in 6–15 minutes.

2. Cross-sectional angiography
CT and MR angiography are essential components of the standard workup for young stroke. Their noninvasive nature, high sensitivity and wide availability allow quick and accurate vascular interpretation. CT angiography, MRI and MR angiography have the advantage over catheter angiography of demonstrating the vessel walls of the larger arteries in the neck in the young population with an increased frequency of dissections. Cross-sectional venous imaging should also be done to rule out cortical venous or dural venous sinus thrombosis.
3. Perfusion Imaging
CT perfusion is a dynamic study yielding a first-pass time-attenuation curve from which perfusion parameters of cerebral blood flow, cerebral blood volume, time to peak, and mean transit time can be calculated. Automated post-processing methods are available, providing volumes of core infarction (cerebral blood flow <30% of normal) and penumbra (time to maximum residual function [Tmax] >6 seconds). It enables the differentiation of salvageable ischemic brain tissue (penumbra) from the irrevocably damaged infarcted brain (infarct core). This is useful when assessing a patient for treatment (thrombolysis/clot retrieval).
4. Vessel wall imaging
Vessel wall imaging (VWI) is a new technique that uses black-blood sequences, pre and post contrast acquisitions to evaluate vessel walls. VWI is used to differentiate between intracranial diseases such as reversible cerebral vasoconstriction syndrome (RCVS), Moya-Moya disease, vasculitis, dissection, and atherosclerosis by evaluating stenosis, eccentric versus concentric nature, location, and enhancement.
5. Catheter Angiography
Indications for catheter angiography include workup for intracranial steno-occlusive diseases like Moya-Moya disease, diagnostic angiography for non-atherosclerotic vasculopathy, and when planning interventions.
CAUSES OF YOUNG STROKE
The most common classification of sub-types of ischemic stroke is the Trial of Org 10172 in Acute Stroke Treatment (TOAST) classification. This scheme divides ischemic strokes into 5 categories which are discussed below.
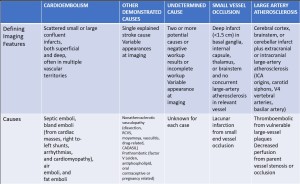
1. Cardioembolic Stroke
They may be categorized on the basis of clot composition or cardiac disease into septic emboli, bland emboli (from cardiac masses, right-to-left shunts, arrhythmias, and cardiomyopathy), air emboli, and fat emboli.
Septic emboli
- Most common intracranial complication in infective endocarditis often associated with intraparenchymal hemorrhage, abscess, subarachnoid hemorrhage, or mycotic aneurysm.
- Occult small embolic stroke (37%) and subcortical micro-hemorrhages (57%) are frequent in asymptomatic patients [4].
Bland emboli
- Most common causes of bland emboli include cardiac tumors like atrial myxoma, right-to-left shunts including patent foramen ovale (37%), arrhythmias like atrial fibrillation and cardiomyopathies.
Intravascular air emboli
-
Cerebrovascular air embolism can occur during many invasive procedures like central venous catheter placement.
-
If the introduction of air is before the branching of aortic vessels, the infarcts are smaller involving multiple vascular territories, while if it's related to a carotid or vertebrobasilar interventional procedure, infarcts are typically confined to a single vascular territory.
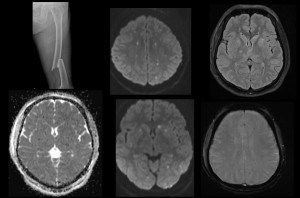
Fat emboli
-
Cerebral fat embolism syndrome is classically seen in patients with large displaced fractures or sickle cell disease [5].
-
Displaced fracture marrow fat droplets released can traverse through a right-to-left cardiac shunt or can deform and travel through intact pulmonary capillary beds to reach the CNS.
- CT is usually normal. The classic“starfield” pattern of innumerable tiny foci of diffusion restriction and FLAIR hyperintensities are noted scattered throughout the brain parenchyma.
2. Other Demonstated Causes
Dissection
-
Cervical carotid or vertebral artery dissection is one of the most common causes of stroke in young adults. They can be spontaneous or traumatic.
-
The mechanism of stroke in patients with carotid dissection includes thromboembolic stroke (80%), hypoperfusion from high grade stenosis or occlusion (15%), and mixed mechanisms (5%).
-
CT angiography can demonstrate a long irregular stenosis (string of pearls sign), tapering of true lumen (flame sign), or mural thickening from intramural hemorrhage.
-
Fat-saturated T1-weighted MRI is the most sensitive imaging modality for depiction of a cervical arterial dissection.

Vasculitis
- Vasculitis is a specific vasculopathy defined as inflammation of the blood vessel wall with or without necrosis.
- The cause of intracranial vasculitis include connective tissue disease or lupus, infection, malignancy, irradiation, or medications. VWI may help identify concentric focal intense wall enhancement, a unique finding indicating inflammation.

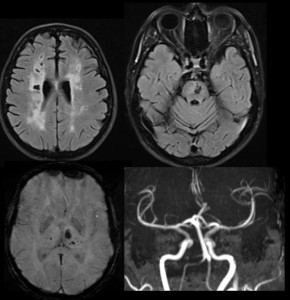
Reversible Cerebral Vasoconstriction Syndrome (RCVS)
RCVS is a combined clinical and radiographic diagnosis of unknown pathophysiology. Subarachnoid hemorrhage in RCVS involves the high convexities instead of the basal cisterns. Multifocal beaded appearance of the larger intracranial vessels in multiple vascular territories is diagnostic of cerebral vasoconstriction but not specific for RCVS. RCVS has no or mild enhancement in VWI, while vasculitis has intense enhancement.
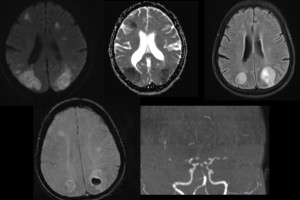
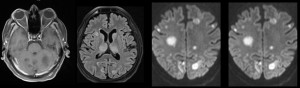
Cerebral autosomal dominant arteriopathy with subcortical infarcts and leukoencephalopathy (CADASIL)
- CADASIL is caused by a genetic mutation in the NOTCH3 gene.
- The typical imaging findings include subcortical and periventricular hyperintense white matter lesions on T2-weighted or FLAIR images involving the anterior temporal poles, insula, centrum semiovale, and external capsule [6]. The lesions are symmetric with relative sparing of the fronto-orbital and occipital regions and associated deep gray matter microhemorrhages.
Moya - Moya
-
Moya-moya disease is idiopathic. Secondary causes of moya-moya syndrome include sickle cell disease, neurofibromatosis type 1, radiation vasculopathy, and Down syndrome.
-
Stroke occurs due to watershed infarction from steno occlusive disease of the ICA terminus that often involves the anterior cerebral artery and MCA origins. Classic “puff of smoke” appearance is seen on angiography.
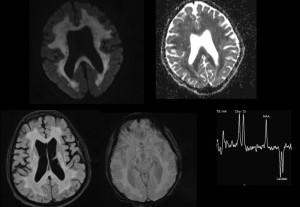
Mitochondrial Encephalopathy, Lactic acidosis and Stroke like episodes (MELAS)
- MELAS is a maternally inherited mitochondrial disorder.
- On imaging, it manifests as multifocal stroke like cortical lesions in different stages of evolution ("shifting spread" pattern), crossing various cerebral vascular territories, and showing a certain predilection to the posterior parietal and occipital lobes.
- Elevated lactate levels are seen on MR spectroscopy.
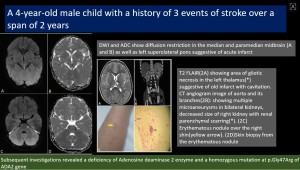
Deficiency of adenosine deaminase 2 (DADA2)
- DADA2 is a monogenic autosomal recessive systemic vasculitis syndrome associated with mutations of ADA2 gene.
- Most common CNS presentation is recurrent strokes due to small vessel lacunar infarcts involving the deep grey matter and brainstem [7].
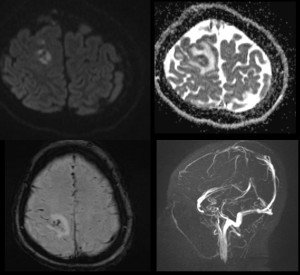
Prothrombotic disorders
- Prothrombotic disorders can induce venous, arterial, or microvascular thrombosis. Some of the causes include Factor V Leiden mutation, antiphospholipid antibody syndrome, oral contraceptive use, pregnancy and puerperium.
- The classic “empty delta sign” or absent cortical venous filling is observed on CT angiography, CT venography, or MR venography.
3. Undetermined causes
Ischemic infarcts due to undetermined causes should meet one of the following criteria: (a) two or more causes, (b) indeterminate cause, and (c) incomplete evaluation[8].
4. Small vessel occlusion
Small-vessel occlusion (lacunar) infarction accounts for only 7%–14% of ischemic strokes in young adults. Imaging features include small deep infarcts restricted to the basal ganglia, internal capsule, thalamus, or brainstem.
5. Large artery atherosclerosis
It's the least common subtype of ischemic infarction in young adults, accounting for only about 2-8%. A stroke can be attributed to large-artery atherosclerosis if the patient has an infarct of the cerebral cortex, brainstem, or cerebellum and evidence of accelerated atherosclerotic risk factors or symptomatic atherosclerosis in other anatomic locations.