CVT is a rare but serious condition that requires rapid diagnosis for early treatment and improved prognosis.
Risk factors: Pregnancy, postpartum, oral contraceptive use, thrombophilia, malignancy, infections, and dehydration.
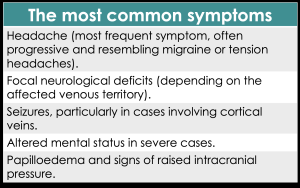
Clinical presentation: The clinical manifestations of CVT can be highly variable and often non specific, which may lead to diagnostic delays. The most common symptoms are described in the table 1.
Given the heterogeneous and sometimes subtle clinical presentation, imaging plays a crucial role in early detection and confirmation of the diagnosis.
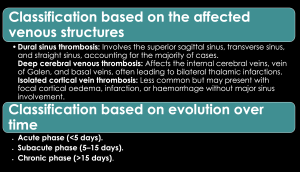
Classification based on the affected venous structures CVT can be classified into three main subtypes based on the affected venous structures.
- Dural sinus thrombosis.
- Deep cerebral venous thrombosis.
- Isolated cortical vein thrombosis.
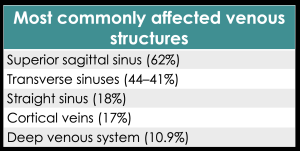
Most commonly affected venous structures
Classification based on evolution over time
CVT can also be classified according to its evolutionary stage:
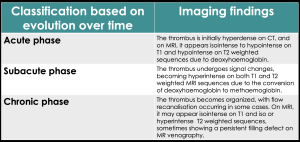
- Acute phase (<5 days).
- Subacute phase (5–15 days).
 Fig 2: Subacute dural sinus thrombosis (A) Axial FLAIR sequence: Hyperintense right sigmoid sinus (arrow) is observed. (B) Sagittal T1 sequence: Hyperintense signal in the right sigmoid sinus (arrow). (C) T1 sequence with gadolinium: Filling defect, findings consistent with subacute right sigmoid sinus thrombosis (arrow).
Fig 2: Subacute dural sinus thrombosis (A) Axial FLAIR sequence: Hyperintense right sigmoid sinus (arrow) is observed. (B) Sagittal T1 sequence: Hyperintense signal in the right sigmoid sinus (arrow). (C) T1 sequence with gadolinium: Filling defect, findings consistent with subacute right sigmoid sinus thrombosis (arrow). - Chronic phase (>15 days).
 Fig 3: Chronic dural sinus thrombosis (A) T1-weighted sequence: Right sigmoid sinus is isointense to the brain parenchyma (arrow). (B) T2-weighted sequence: Right sigmoid sinus is isointense to the brain parenchyma (arrow). (C) T1-weighted sequence with gadolinium: Filling defect, findings consistent with chronic right sigmoid sinus thrombosis (arrow).
Fig 3: Chronic dural sinus thrombosis (A) T1-weighted sequence: Right sigmoid sinus is isointense to the brain parenchyma (arrow). (B) T2-weighted sequence: Right sigmoid sinus is isointense to the brain parenchyma (arrow). (C) T1-weighted sequence with gadolinium: Filling defect, findings consistent with chronic right sigmoid sinus thrombosis (arrow).