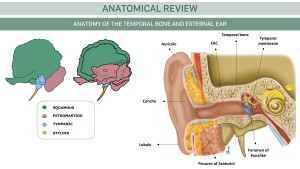
1. Anatomy of the External Ear
The temporal bone is a complex structure requiring detailed knowledge of its relationships with surrounding bony, neural, muscular, and vascular elements.
The temporal bones comprise the lateral skull base, forming portions of the middle and posterior fossae. Each temporal bone consists of five osseous parts: squamous, mastoid, petrous, tympanic, and styloid.
The external ear includes the auricle and the EAC, ending at the tympanic membrane.
The auricle consists of an irregular concave plate of elastic cartilage and dense connective tissue, covered by skin containing hairs, sebaceous, and ceruminous glands.
The external auditory canal (EAC) is an S-shaped tube within the tympanic portion of the temporal bone. It measures approximately 3 cm and extends from the auricle to the tympanic membrane. The anterior wall forms the posterior face of the glenoid fossa, while the posterior wall forms the anterior margin of the mastoid.
- Lateral one-third: fibrocartilaginous covered by thicker skin. On its anterior margin lie the fissures of Santorini, a potential pathway for the spread of infection/neoplasms, between the parotid, TMJ, and the EAC.
- Medial two-thirds: surrounded by the tympanic portion of the temporal bone. A defect in the anteroinferior surface of the bony canal connecting to the TMJ is called the foramen tympanicum (Huschke's foramen).
- Isthmus: narrowest part of the EAC, located at the bony-cartilaginous junction.
The tympanic membrane is a thin, obliquely oriented membrane approximately 10 mm in diameter. It consists of two parts: the larger pars tensa (anteroinferiorly), composed of fibrous material, and the pars flaccida (posterosuperiorly), more prone to perforation due to its collagen fiber composition.
2. Imaging of the temporal bone and EAC
CT and MRI are the key diagnostic modalities used to evaluate EE lesions, playing complementary roles in the diagnosis.
Computed tomography (CT)
First-line imaging for high-resolution bone detail, surgical planning, and urgent pathology evaluation. Contrast is reserved for vascular, infectious, or neoplastic concerns.
- Volumetric acquisition in the axial plane with a bone filter and a slice thickness of 0.6–0.8 mm.
- Bone and soft tissue algorithms.
- The scan should extend from the skull base (mastoid tip) to the arcuate eminence/orbital roof.
Reconstructions are performed in axial and coronal planes with the same slice thickness. Additional projections include:
- Oblique-longitudinal projection (Stenvers view): Parallel to the long axis (perpendicular to the superior semicircular canal). Evaluation: short axis of the cochlea, vestibular aqueduct, facial nerve, round window, and incudomalleolar joint.
- Oblique-transverse projection (Pöschl view): Perpendicular to the long axis (parallel to the superior semicircular canal). Evaluation: superior semicircular canal, long axis of the cochlea, bony vestibular aqueduct, and the "two-window view".
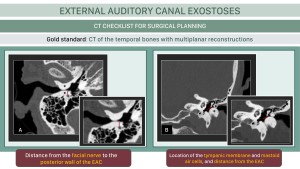
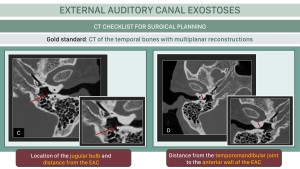
 Fig 2: HELICAL CT OF THE TEMPORAL BONE. In the preoperative study of the EAC, should be assessed: morphology of auricle and soft tissues (a), EAC Caliber (b), tympanic membrane (c), distance from the posterior wall of the EAC to the 3º portion of the Facial Canal (d), distance from the anterior wall of the EAC to the TMJ (e).
Fig 2: HELICAL CT OF THE TEMPORAL BONE. In the preoperative study of the EAC, should be assessed: morphology of auricle and soft tissues (a), EAC Caliber (b), tympanic membrane (c), distance from the posterior wall of the EAC to the 3º portion of the Facial Canal (d), distance from the anterior wall of the EAC to the TMJ (e).
Cone beam CT (CBCT)
CBCT is a variant of conventional CT that acquires a volumetric dataset in a single rotation using a divergent cone-shaped X-ray beam and 2D detectors. It offers high-resolution bone imaging with lower radiation but limited soft tissue assessment.
- Evaluation of the ossicular chain, bony labyrinth, cochlear anatomy, and facial nerve.
- Postoperative assessment of middle ear and cochlear implants, minimizing metal artifacts.
- Detection of ossicular chain erosions and intraoperative surgical guidance for temporal bone procedures.
 Fig 3: CBCT OF THE TEMPORAL BONE. In the preoperative study of the EAC, should be assessed: morphology of auricle and soft tissues (a), EAC Caliber (b), tympanic membrane (c), distance from the posterior wall of the EAC to the 3º portion of the Facial Canal (d), distance from the anterior wall of the EAC to the TMJ (e).
Fig 3: CBCT OF THE TEMPORAL BONE. In the preoperative study of the EAC, should be assessed: morphology of auricle and soft tissues (a), EAC Caliber (b), tympanic membrane (c), distance from the posterior wall of the EAC to the 3º portion of the Facial Canal (d), distance from the anterior wall of the EAC to the TMJ (e).
MRI
MRI is more specific for distinguishing tumors from inflammatory lesions and better defines malignant neoplasm extension, including perineural spread.
Anatomical References and Radiological Planes in Preoperative Evaluation
Preoperative CT assessment provides extensive information, including determining the extent of the disease, identifying anatomical variants, detecting congenital or acquired anomalies, and preventing potential complications. In the preoperative study of the EAC, the following aspects should be assessed:
- Auricle and Soft Tissues (axial/coronal): morphology.
- EAC Caliber (axial/coronal): Height 0.91–0.96 cm, width 0.63–0.67 cm, and length 2.5 cm. Evaluate patency and rule out obstructions.
- Tympanic Membrane (coronal): thickening, perforation, or retraction.
- Distance from the Posterior Wall of the EAC to the third portion of the Facial Canal (axial): 5.53 ± 1 mm.
- Distance from the anterior wall of the EAC to the TMJ (axial).
3. EAC exostoses (EAE)
Surfer’s ear or external auditory exostoses is a slow-progressing benign and irreversible bone growth within the EAC resulting from chronic cold water or wind exposure.
Repeated cold exposure induces bone growth at the tympanic ring through a process that involves vasodilation and inflammation, leading to periostitis and osteoblast activity.
Presentation: EAC exostosis, usually asymptomatic, serves as a protective mechanism. It can cause conductive hearing loss, aural fullness, and otalgia from otitis externa, cerumen impaction, tympanic membrane rupture, or water trapping.
Otoscopy: Firm, nodular formations causing epithelial atrophy and potential canal obstruction. Exostoses are typically multiple, bilateral, and medial to the isthmus, located anteriorly and posteriorly. The otoscopic grading ranges from 0 (No exostosis) to 3 (>67% obstruction) and determines management.
Audiometry: mandatory in the preoperative assessment. Often normal; may reveal an air-bone gap (7–15 dB). Complete canal obliteration can cause up to 60 dB conductive loss.
CT: gold standard in diagnosis, severity grading, and surgical planning. These benign outgrowths appear as dense bilateral broad-based protuberances on the osseous EAC, medial to the isthmus. CT is critical for preoperative assessment:
- Assessing medial extension relative to the tympanic annulus.
- Mapping of the Facial Nerve Pathway near the posterior tympanic frame to prevent surgical complications
- Ruling out concomitant Middle Ear pathology.
 Fig 4: EXTERNAL AUDITORY CANAL EXOSTOSES. Bilateral broad-based bony overgrowth arising from the roof, anterior and posterior walls of the osseous EAC, with significant stenosis in the innermost part of both bony EAC.
Fig 4: EXTERNAL AUDITORY CANAL EXOSTOSES. Bilateral broad-based bony overgrowth arising from the roof, anterior and posterior walls of the osseous EAC, with significant stenosis in the innermost part of both bony EAC.
There are certain measurements to consider in the surgical planning CT.
Management is conservative in mild cases. In moderate to severe exostoses or recurrent/persistent symptoms, surgical intervention may be considered.
4. Differential diagnosis
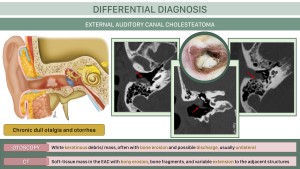
Cholesteatoma
Lesion containing defoliating keratin lined by keratinizing stratified squamous epithelium with periostitis and bone erosion.
Presentation: chronic otalgia, otorrhea, and sometimes conductive hearing loss due to canal occlusion.
Otoscopy: White keratinous mass with EAC erosion, localized in the inferior or posterior wall, where keratin debris, granulation tissue, and sequestrated bone are present.
CT: soft-tissue mass in the EAC with bony erosion, bone fragments, and extension to adjacent structures. Deep extension into the middle ear, mastoid air cells, facial nerve canal, or tegmen tympani must be reported.
MRI: diffusion restriction, confirming the diagnosis.
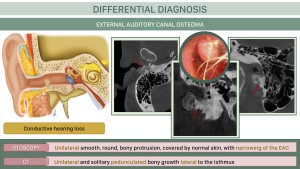
Osteoma
Rare focal pedunculated bony overgrowths of the osseous EAC, that can cause conductive hearing loss.
Histopathologically, osteomas are composed of fibrovascular channels surrounded by dense cortical bone with a laminar pattern, unlike the appositional growth of compact bone in exostoses.
Presentation: asymptomatic / conductive hearing loss
Otoscopy: Unilateral smooth, round bony protrusion covered by normal skin, narrowing the EAC.
CT: hyperattenuating and solitary pedunculated bony growth lateral to the isthmus, at the tympanosquamous and tympanomastoid sutures.
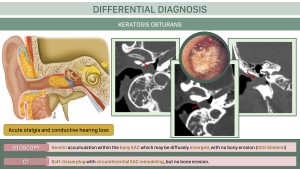
Keratosis obturans
Abnormal keratin accumulation causing bony EAC occlusion and expansion, linked to cerumen gland overstimulation or epithelial dysregulation.
Histopathologically similar to cholesteatoma, without focal osteonecrosis.
Presentation: acute severe pain and conductive hearing loss.
Otoscopy: keratin accumulation in an enlarged bony EAC, without bony erosion.
CT: soft-tissue plug in the EAC with canal expansion due to remodeling, but no bone erosion, as opposed to cholesteatoma, bilateral in 50% of cases.
MRI: features overlap with cholesteatoma.
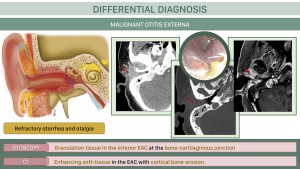
Malignant otitis externa
Invasive infection of the EAC which can spread rapidly to the surrounding soft tissue, neck spaces, and skull base, commonly in diabetics and immunosuppressed patients. P. aeruginosa is the main pathogen.
Presentation: persistent otorrhea and otalgia, refractory to standard treatment.
Otoscopy: erythema, edema and granulation tissue in the anterior or inferior walls of the EAC at the bone-cartilaginous junction. Crusting, necrotic debris, or exposed bone appear in advanced cases.
CT: enhancing soft-tissue thickening in the EAC with cortical bone erosion and potential phlegmon/abscess formation. Potential complications include skull base or TMJ osteomyelitis with potential intracranial spread of infection via fissures of Santorini.
MRI: superior for assessing soft tissue, bone marrow involvement, intracranial extension and cranial nerve involvement.
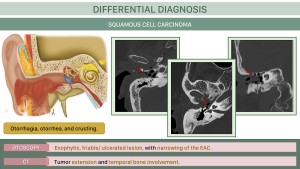
Squamous cell carcinoma
The most common primary malignant EAC tumor, characterized by the abnormal growth of squamous cells, associated with chronic inflammation and prior radiation.
Presentation: otorrhagia, persistent otorrhea, and crusting.
Otoscopy: exophytic, friable, or ulcerated lesion, with associated canal stenosis and anatomical distortion.
CT: Contrast-enhanced CT is key for assessing tumor extent, bone destruction, and soft tissue involvement.
Differential diagnosis with malignant external otitis and cholesteatoma is challenging, making clinical correlation and histopathological diagnosis essential (cholesteatoma shows higher diffusion restriction).