
- Patient Characteristics
A total of 170 patients (mean age, 66.6 ± 13.0 years; 72 males and 98 females) were included. No significant differences were observed between groups in demographic characteristics or contrast injection parameters. Within the CO₂ insufflation group, colonic gas volume did not differ significantly among scan-delay subgroups.
- IMV Enhancement
The IMV demonstrated a clear shift in enhancement timing depending on CO₂ insufflation.
CO₂ insufflation group
- The highest IMV attenuation was observed at a 25-second delay (283.0 ± 40.4 HU).
- Attenuation decreased significantly at 30 and 35 seconds (p < 0.001).
Non-insufflation group
- Peak enhancement occurred at 30–35 seconds (p = 0.002).
- The 25-second delay yielded the lowest IMV attenuation.
These findings indicate that CO₂ insufflation is associated with an earlier peak arrival of contrast enhancement in the IMV.
- SMV Enhancement
The SMV also exhibited earlier enhancement with CO₂ insufflation, although the effect was less pronounced than that observed in the IMV.
CO₂ insufflation group
- Maximum SMV attenuation was observed at 25 seconds (247.0 ± 37.1 HU).
- Attenuation declined at longer delays (p < 0.001).
Non-insufflation group
- No distinct shift in peak timing was observed.
- Enhancement remained relatively stable across scan delays.
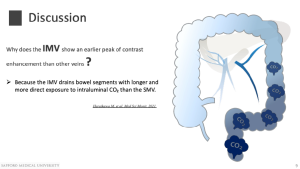
This difference reflects anatomical drainage patterns: the IMV drains bowel segments directly exposed to CO₂, whereas the SMV primarily drains the small intestine and right colon.
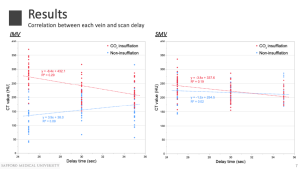
- Correlation Between Scan Delay and Venous Enhancement
Correlation analysis demonstrated contrasting enhancement dynamics:
- IMV (CO₂ insufflation group): strong negative correlation (r = –0.54, p < 0.001).
- IMV (non-insufflation group): positive correlation (r = 0.30, p = 0.007).
- SMV (CO₂ insufflation group): moderate negative correlation (r = –0.44, p < 0.001).
These findings indicate that CO₂ insufflation is associated with a steeper and earlier enhancement curve, whereas absence of CO₂ results in delayed venous opacification.
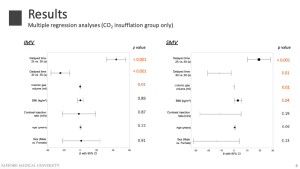
- Multivariate Analysis (CO₂ Insufflation Group)
Multivariate linear regression analysis within the CO₂ insufflation group demonstrated that both scan delay and colonic gas volume were significant negative predictors of mesenteric venous enhancement in the IMV and SMV.
- Colonic gas volume showed a clear inverse relationship with venous attenuation.
- Larger intraluminal gas volumes, reflecting greater colonic distension, were associated with lower enhancement in both veins.
These findings suggest that excessive colonic distension may transiently increase intraluminal or intra-abdominal pressure, thereby reducing venous return and attenuating contrast opacification. Sex, age, and contrast injection rate were not significant predictors.
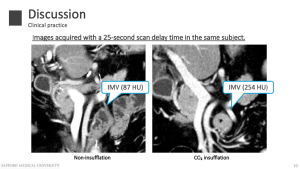
- Qualitative Visual Comparison
Qualitative visual comparison supported the quantitative findings. At a 25-second delay, IMV enhancement was more homogeneous and conspicuous in CO₂-insufflated examinations. In contrast, without CO₂ insufflation, venous structures appeared less distinct and required longer scan delays for comparable opacification. These differences have practical implications for preoperative vascular mapping and EMVI assessment.
Discussion
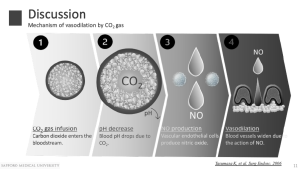
Physiological Mechanisms
Earlier venous enhancement observed in the CO₂ insufflation group is consistent with previously reported physiological effects of CO₂ insufflation [8,9]:
- Rapid mucosal absorption of CO₂.
- Increased local pCO₂ and mild tissue acidosis.
- Nitric oxide–mediated vasodilation.
- Increased splanchnic perfusion.
- Accelerated venous return.
The IMV demonstrates the strongest response because it drains bowel segments directly exposed to intraluminal CO₂.
Clinical Implications
Key clinical implications include:
- Optimal mesenteric venous visualization with CO₂ insufflation occurs at approximately 25 seconds, earlier than conventional portal venous timing.
- Improved IMV opacification may enhance detection of EMVI and facilitate safer surgical planning.
- Excessive CO₂ distension may paradoxically reduce venous enhancement, underscoring the importance of balanced insufflation rather than maximal inflation.
These findings support a tailored CT colonography protocol that integrates insufflation strategies with optimized scan timing.
Limitations
This study is limited by its retrospective design, heterogeneity of underlying diseases in the non-insufflation group, and evaluation restricted to three fixed scan delays. Variability in colonic CO₂ volume may also influence hemodynamic responses.