Our study will focus only on cystic non ovarian intraperitoneal lesions of the Pelvis (1):
1- Differentiate the non-ovarian cystic lesions: First crucial step to do!
1A-Imaging Techniques and Diagnostic Criteria:
1.MRI:
- Superior contrast resolution and multiplanar capability.
- Key for distinguishing ovarian from non-ovarian lesions.
- Challenges include overlapping appearances and ovary displacement due to large masses or postpartum changes.
2.CT:
- Useful in characterizing calcifications, density, and acute pathologies such as appendiceal mucoceles or pelvic abscesses.
1B-Key Imaging Signs:
- Ovarian Origin:
- Suspensory ligament sign (ovarian vein visualization).
- Crescent-shaped ovarian parenchyma.
- Mesosalpinx displacement patterns.
- Non-Ovarian Lesions: (fig1)
- Tubal: Hydrosalpinx shows a tubular shape with incomplete partitions.
- Uterine: Presence of a pedicle or “spur sign”.
- Extraperitoneal: Displacement of adjacent urogenital structures.
2- Recognize the final pathology and describe it with MRI and/or CT:
2A. Cystic Lesions of Peritoneal Origin:
a.Peritoneal Inclusion Cysts (PIC)
Also called Peritoneal pseudocysts.
- Cause: reactive mesothelial proliferation due to peritoneal insult (e.g., endometriosis,pelvic inflammatory disease...).
- Common in premenopausal women with active ovaries and pelvic adhesions.
- They may recur. (2)
- MRI: High T2 signal, thin walls conforming to the peritoneum.
- CT: Multilocular hypodense structures.
Ps: Hydrosalpinx can mimic PIC but has a more tubular appearance, and loculated ascites which is usually found in the most dependent portions of the peritoneal cavity.
b.Para ovarian cysts
- Commonly observed in women during their third and fourth decades of life.
- Bilateral occurrence or multiple unilateral cysts have been documented.
- Potential complications: Torsion, haemorrhage, or rupture. Rarely, neoplastic changes can develop within these cysts. (3) (4)
Paraovarian cysts arise from the broad ligament, the adjacent ovary remains unaffected and retains its normal morphology
- No specific CT or MRI features that reliably differentiate paraovarian cysts from ovarian cysts.
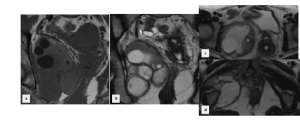
- MRI: Homogeneous high signal on T2-weighted images, low signal on T1-weighted images. Hemorrhagic cysts show high signal intensity on T1. (Fig2)
- CT: Thin-walled, separate from the ovary.
 Fig 2: MRI- T1(a),T2 (b,c),T1 gado: unilocular cystic mass inter-utero-rectal in the Douglas push The ovaries were seen in their dimples (arrow) ; histologic diagnosis (para-adnexal cyst)
Fig 2: MRI- T1(a),T2 (b,c),T1 gado: unilocular cystic mass inter-utero-rectal in the Douglas push The ovaries were seen in their dimples (arrow) ; histologic diagnosis (para-adnexal cyst)
c.Pseudo-Myxoma Peritonei (PMP)
2B. Cystic lesions of appendiceal origin:
a.Mucocele of the Appendix
- Rare condition due to an obstructed, dilated appendix filled with mucin.
- It’s important to identify a mucocele preoperatively to prevent rupture at surgery which may result in the development of Pseudomyxoma Peritonei, and also to predict malignant transformation. (5)
- MRI: High T2 signal, possible wall nodules. (fig3)
- CT: Well-defined cystic mass with possible calcifications.
 Fig 3: Left latero-uterine formation with liquid content, serpiginous tubular structure, seat of incomplete septas (“Waist sign”) enhanced after injection, without bud or parietal nodules: Hydrosalpinx Right pelvic oblong pear-shaped formation, liquid content with nodular parietal thickening enhanced after injection, appended to ruptured caecal fundus with small pelvic effusion: ruptured appendicular mucocele.
Fig 3: Left latero-uterine formation with liquid content, serpiginous tubular structure, seat of incomplete septas (“Waist sign”) enhanced after injection, without bud or parietal nodules: Hydrosalpinx Right pelvic oblong pear-shaped formation, liquid content with nodular parietal thickening enhanced after injection, appended to ruptured caecal fundus with small pelvic effusion: ruptured appendicular mucocele.
Ps: The most common tumors leading to PMP are appendicular and ovarian mucinous tumors. PMP is another mimic of non-ovarian cystic lesions of the pelvis. It’s considerate from peritoneal origin.
2C. Cystic Lesions of Fallopian Tube Origin:
a.b.c. Hydrosalpinx, Pyosalpinx, and Hematosalpinx
Dilated fallopian tubes filled with fluid (Hydrosalpinx), pus (Pyosalpinx), or blood (Hematosalpinx).
Common causes: pelvic inflammatory disease (PID), endometriosis, ectopic pregnancy.
a.Hydrosalpinx
- The most distinctive and useful features of hydrosalpinx are: Tubular structure with “waist sign”: indicative of a constricted segment. (6)
- MRI: High T2 signal; CT shows fluid-filled tubular masses. (fig3)
b.Hematosalpinx
- Commonly seen within the context of endometriosis but a tubal ectopic pregnancy (Fig4) , adnexal torsion, malignancy or trauma can also cause bleeding within the fallopian tube.
- MRI: High signal intensity on T1 fat-sat images: blood products.
c.Pyosalpinx
- Commonly caused by Neisseria Gonorrhea or Chlamydia Trachomatis but in 30-40% of cases it has a polymicrobial cause.
- Likely it’s bilateral.
- CT/MRI: Thick-walled (differentiate it from Hydrosalpinx), fluid-filled adnexal mass with signs of inflammation: Thickened uterosacral ligaments and infiltration of presacral fat.
d.Ectopic pregnancy
Case highlight section 1
Ectopic pregnancies, particularly chronic cases, can closely mimic peritoneal cysts due to their cystic appearance and anatomical location.
This condition most commonly involves the fallopian tubes and can present diagnostic challenges without careful clinical and imaging correlation. (7)
- US is the mainstay of diagnosis, but MRI and CT may be useful adjuncts in cases of diagnostic doubt.
- MRI: Demonstrates heterogeneous cystic lesions with a thickened wall. High T1 signal (subacute hemorrhage) and low T2 signal (acute or subacute hemorrhage) are characteristic findings. The presence of trophoblastic tissue or a gestational sac aids differentiation. (As shown in fig4: A rare case of chronic ectopic pregnancy in a 29 year-old woman, admitted with subacute pelvic pain. MRI showed an empty uterus with normal ovaries. )
- CT: Shows complex adnexal masses, hemoperitoneum, or hematosalpinx, which may be misinterpreted as encapsulated peritoneal cysts. Advanced imaging allows precise localization and identification of tubal origin.
 Fig 4: Axial T2-weighted MR image shows masses of high and medium signal intensity and axial T1-weighted MR image shows the same masses with medium signal intensity suggesting an encysted hematocele. Axial T1-weighted MR image shows also a cystic gestational sac (GS) with a yolk-like structure surrounded by a thick wall. Post-contrast axial T1-weighted MR image shows a sausage like structure with an enhancing wall corresponding to the right fallopian tube that contains the GS surrounded by the trophoblast.
Fig 4: Axial T2-weighted MR image shows masses of high and medium signal intensity and axial T1-weighted MR image shows the same masses with medium signal intensity suggesting an encysted hematocele. Axial T1-weighted MR image shows also a cystic gestational sac (GS) with a yolk-like structure surrounded by a thick wall. Post-contrast axial T1-weighted MR image shows a sausage like structure with an enhancing wall corresponding to the right fallopian tube that contains the GS surrounded by the trophoblast.
Ps: Chronic ectopic pregnancies should always be considered in cases of atypical pelvic cysts, especially in patients with a history of pelvic inflammatory disease or infertility treatments.
2D. Cystic lesions of Uterine origin:
a.Degenerating Leiomyoma
- Benign tumors of uterine smooth muscle. (8)
- 2/3 of leiomyomas over 5-8cm show some form of degeneration.
- MRI: T2 hyperintense degeneration; bridging vessel sign linking the lesion to the myometrium.
- CT: Hypodense with calcifications or hemorrhagic changes. (8)
- Contrast enhancement can be minimal or variable, reflecting the extent of necrosis or vascularity. (fig5)
 Fig 5: Posterior corporeo-fundial myoma, interstitial and subserous, heterogeneous spontaneous and enhancement density: Complicated myoma
Fig 5: Posterior corporeo-fundial myoma, interstitial and subserous, heterogeneous spontaneous and enhancement density: Complicated myoma
b.Cystic Adenomyosis
- Histologically-defined as the presence of ectopic endometrial tissue within the myometrium.
- There are 3 forms of adenomyosis: Diffuse adenomyosis, focal adenomyosis and cystic adenomyosis.
- Common, non-neoplastic condition which affects menstruating women.
- MRI: high signal intensity on T1-weighted fat-Sat, intermediate to high signal intensity on T2. It can demonstrate low signal intensity on T2- weighted imaging from hyaline degeneration of the hyperplasic smooth muscle and therefore can be indistinguishable from hyaline degeneration of a leiomyoma.
Ps: Hemorrhagic degeneration of a leiomyoma can also give the same characteristics as the blood filled adenomyotic cyst.
c.Unicornuate uterus with obstructed horn
- Developmental anomaly where a rudimentary horn becomes dilated and filled with fluid or blood.
- MRI: High T2 signal intensity; low T1 signal for chronic blood.
f.Isthmocele
- A cesarean scar defect. (9)
- MRI: Fluid-filled pouch in the anterior lower uterine segment, often connected to the endometrial cavity, with T2-hyperintense and T1-hypointense signals.
- CT: Cystic lesion in the lower uterine segment. Its location near the cesarean scar and continuity with the endometrial cavity helps differentiate it from ovarian cysts. (as shown in fig6)
 Fig 6: Uterus of normal size, homogeneously raised, with an intramyometrial formation opposite the hysterorrhaphy scar communicating with the uterine cavity, well-limited round shape, hypodense, raised wall: Isthmocele
Fig 6: Uterus of normal size, homogeneously raised, with an intramyometrial formation opposite the hysterorrhaphy scar communicating with the uterine cavity, well-limited round shape, hypodense, raised wall: Isthmocele
2E. Intra and extra peritoneal masses:
a.Pelvic Abscess
- Often arise from appendicitis, diverticulitis, or post-surgical infections.
- Imaging shows thick-walled collections with inflammatory changes.
b.Hematomas
- Result from trauma or coagulopathy.
- CT demonstrates hyperdense acute collections; chronic hematomas appear hypodense.
c.Lymphoceles
- Post-surgical collections, commonly after lymphadenectomy.
- CT/MRI: Typically appear as thin-walled, fluid-filled structures.
d.Bladder Diverticula
- Protrusions from the bladder wall, occasionally misidentified as pelvic cysts.
- Imaging reveals a connection to the bladder lumen.
2F. Case highlight section 2:
A rare case of a sub-peritoneal pelvic hydatid cyst presented as a significant diagnostic challenge due to its close resemblance to an ovarian complicated cyst. (10)
- Advanced imaging techniques, including MRI and CT, revealed characteristic features such as daughter cysts with high T2 signal intensity surrounded by a low-signal intensity capsule, and a well-defined cystic mass with possible calcifications.
- In ruptured cases, the presence of floating laminated membranes, known as the 'water-lily sign,' further aids diagnosis.
This case underscores the necessity of considering hydatid disease in the differential diagnosis of pelvic cystic masses, particularly in endemic regions, where overlooking this possibility could lead to delayed or inappropriate management. (eg : fig7: Sub peritoneal multilocular cyst in the right ischio-anal fossa having been mistaken in a first evaluation by ultrasound for ovarian cystic mass when it was an hydatic cyst of the ischio-anal fossa.)