The clinical manifestations associated with these syndromes are heterogeneous, often mediated through the action of cytokines, hormones, or immune cross-reactivity. This presentation utilizes radiological images sourced from our institution to elucidate the underlying radiographic findings characterizing these paraneoplastic syndromes.
Drawing from our clinical experience, we have encountered several paraneoplastic syndromes, including:
Neurological syndromes:
- Anti-GABAAR Encephalitis:
Antibodies targeting the ALFA1 and β3 subunits of this receptor are linked to seizures and status epilepticus in cases of autoimmune encephalitis. Symptom prevalence and associated conditions vary between children (often post-viral) and adults (typically tumor-related). Roughly 40% of adult patients exhibit an underlying tumor, commonly a thymoma.
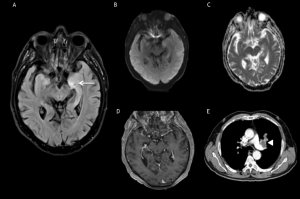
On MRI scans, most patients show extensive multifocal involvement, with multiple areas of hyperintensity on T2/FLAIR sequences with unilateral or bilateral distribution, affecting cortex and subcortical white matter. These areas rarely show contrast enhancement. Their manifestation occurs asynchronously, occasionally unrelated to symptoms. This MRI presentation is uncommon in other forms of autoimmune encephalitis and serves as a diagnostic key.
Multifocal brain lesions detected on MRI may originate from diverse underlying causes, including but not limited to tumors, demyelinating disorders, infections, mitochondrial encephalomyopathy, and stroke-like episodes. Consequently, correct differential diagnosis is challenging.

- Limbic encephalitis:
Limbic encephalitis (LE) is a PNS that usually manifests with seizures, short-term memory loss, confusion, and psychologic dysfunctions that rapidly progress. Its etiology frequently stems from an underlying neoplasm, predominantly small cell lung cancer (SCLC), detected in approximately 55% of LE cases, often correlated with the presence of anti-Hu antibodies. LE has also been observed in connection with testicular, gastrointestinal or breast cancers. Anti NMDA receptor antibodies are usually found in LE in young women and are strongly associated with tumors, particularly with mature and immature ovarian teratomas. Despite LE can manifest independently of a paraneoplastic syndrome, its robust association with malignancy necessitates thorough investigation for underlying tumors.
On MR images, the earliest visible changes of LE appear as hyperintense signal with FLAIR and T2 weighted sequences, typically involving the medial temporal lobes and limbic structures. Patchy areas of enhancement can be seen. True diffusion restriction and hemorrhage are not common and suggest alternative diagnoses.
Differential diagnosis includes herpes simplex virus encephalitis, postictal changes, or low-grade tumors of the central nervous system.
Endocrine syndromes:
- McKittrick-Wheelock syndrome:
This uncommon condition is characterized by profuse secretory diarrhea, wich can progress to severe and lead to fluid and electrolyte imbalances due to a hypersecretory colorectal villous adenoma. Lesions of larger size and distal placement might elevate the likelihood of progressing to this syndrome, potentially due to a diminished ability of the bowel to reabsorb secretions. Villous lesions are advanced adenomas that have malignant potential that occur most commonly in the rectum and they typically remain asymptomatic.
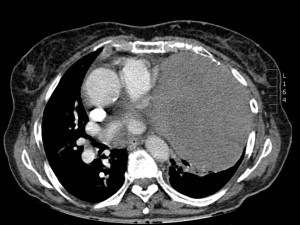
Radiological modalities such as CT scans, CT colonography, and MRI serve as essential tools for visualizing these lesions, revealing large lobulated soft-tissue masses within the luminal space. These imaging techniques occasionally detect associated complications such as intussusception or obstruction.
Distinguishing villous lesions from other endorectal pathologies often necessitates histological analysis of biopsy samples obtained procured during colonoscopy.

- Cushing syndrome:
Approximately 5%–10% of cases of Cushing syndrome, or hypercortisolism, are considered to be of paraneoplastic origin, with nearly 50% of these cases linked to neuroendocrine lung tumors (such as SCLC and bronchial carcinoids). This syndrome can also arise from neuroendocrine tumors located in the thymus, adrenal glands, or gastrointestinal tract.
Cushing's syndrome often exhibit a rapid onset of symptoms, including hypertension, muscle weakness, signs of hypokalemia, and generalized edema. The prognosis is adversely affected by the immunosuppressive effects resultant from hypercortisolism. Failure to suppress cortisol levels with high-dose dexamethasone confirms the presence of ectopic paraneoplastic syndrome.
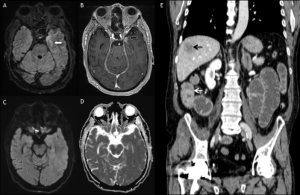
Regarding the diagnosis, imaging examinations are required to locate the primary tumor and rule out a pituitary or adrenal lesion. Nuclear medicine imaging techniques can aid in diagnosis, sometimes revealing cases not detected by other imaging methods.

- Doege-Potter syndrome:
This condition arises as a rare paraneoplastic manifestation associated connected with solitary fibrous tumors (SFTs). It manifests as hypoinsulinemic hypoglycemia due to the abnormal secretion of insulin-like growth factor II (IGF-II) prohormone by these tumors.
Symptoms include confusion, drowsiness, inappropriate sweating, and low blood glucose levels, necessitating the presence of these signs for diagnosis alongside the detection of prohormone IGF-II secretion. The resultant hypoglycaemia can be fatal if definitive surgical intervention is not performed.
SFTs are mesenchymal neoplasms whose origin is not definitively known; although they commonly arise in the thoracic region, extrathoracic cases exist. Computed tomography (CT) is highly valuable in diagnosing intrathoracic SFTs, while magnetic resonance imaging (MRI) aids in better delineating tumor boundaries and relationships with surrounding tissue. However, confirming an SFT requires histological identification through biopsy or surgical resection.
The differential diagnosis of SFTs is broad and depends on their location, emphasizing the need for a comprehensive evaluation involving clinical, imaging, and histological assessments to distinguish SFTs from other similar conditions or tumors.
- Humoral hypercalcemia of malignancy (HHM):
This situation manifests in approximately 10% of patients with advanced tumors and often signifies a poor prognosis. The clinical presentation of includes symptoms such as nausea, vomiting, cognitive impairment, polyuria, renal dysfunction, and in severe cases, coma. The severity of these symptoms correlates with the extent of hypercalcemia, the speed of its onset, and the patient's baseline renal and neurological function. The most commonly tumor associatd with HHM is squamous cell carcinoma, although osteosarcoma, small cell lung carcinoma (SCLC), Hodgkin lymphoma, and various renal and gynecologic malignant tumors have also been reported.
Before considering an HHM diagnosis, it´s imperative to initially rule out benign causes such as sarcoidosis and hyperparathyroidism. In approximately 80% of HHM cases, the primary tumor secretes parathyroid hormone- related protein.
To evaluate HHM comprehensively, employing a multimodal imaging approach is recommended. This aids in identifying the primary tumor and assessing its characteristics, facilitating a more precise diagnosis and appropriate management.
Reumatological:
- Hipertrophic osteoartropathy (HOA):
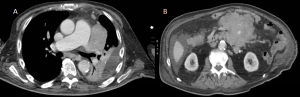
This entitity expresses as chronic periosteal proliferation along long bones and digital clubbing, caused by ectopic growth hormone and vascular endothelial growth factor production, in the absence of an underlying bone lesion. While primary HOA is a rare genetic disorder, secondary HOA prevails as the predominant form (95-97% of HOA cases).
Commonly associated malignancies include pleural mesothelioma and non-small cell lung carcinomas (non-SCLCs), yet benign etiologies like aortic aneurysms, endocarditis, patent ductus arteriosus, or pleural solitary fibrous tumors also induce HOA.
Clinical presentations of HOA vary widely, ranging from asymptomatic cases to manifestations of arthralgia and bone pain.
Plain radiography should be the first imaging modality performed, wich will show metaphyseal and diaphyseal smooth periosteal reaction in long bones. Soft-tissue anomalies, such as finger deformities and aberrant nail curvatures, may also be evident. Magnetic resonance imaging (MRI) aids in assessing muscle and bone marrow edema, while bone scintigraphy stands as the most sensitive diagnostic test for HOA.
The differential diagnosis for HOA includes a wide range of conditions, such as leukemia, lymphoma, venous stasis, and voriconazole-induced periostitis.
