Congress:
ECR25
Poster Number:
C-12335
Type:
Poster: EPOS Radiologist (educational)
DOI:
10.26044/ecr2025/C-12335
Authorblock:
A. Fornaro, F. Donati, D. Cioni, E. Neri; Pisa/IT
Disclosures:
Antonio Fornaro:
Nothing to disclose
Francescamaria Donati:
Nothing to disclose
Dania Cioni:
Nothing to disclose
Emanuele Neri:
Nothing to disclose
Keywords:
Abdomen, Pancreas, MR, MR-Cholangiography, Contrast agent-intravenous, Cysts, Neoplasia
The WHO classifies cystic pancreatic lesions into non-neoplastic and neoplastic epithelial forms. Radiologically, PCNs are categorized based on their communication with the main pancreatic duct.
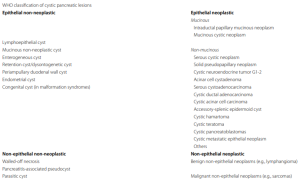
Table 1: WHO classification of cistyc pancreatic lesions.
Morana, G., Ciet, P. & Venturini, S. Cystic pancreatic lesions: MR imaging findings and management. Insights Imaging 12, 115 (2021). https://doi.org/10.1186/s13244-021-01060-z
Common PCNs
1. Serous Cystadenoma (SCA)
- Predominantly affects women (fifth to seventh decade, ‘grandmother lesion’)
- Sporadic occurrence; rarely associated with von Hippel-Lindau (VHL) syndrome
- Can localize anywhere in the pancreas, most commonly in the head
- Typically asymptomatic but can cause obstructive pancreatitis if large
- Macroscopic forms: microcystic (most common), cluster of microcysts (<2 cm) forming a honeycomb pattern; oligocystic (macrocystic), larger (>2 cm) locules, mimicking other tumors; pseudosolid appears as a homogeneous, capsular nodule, resembling a solid lesion
- Pathognomonic feature: centrolesional scar
 Fig 1: Serous Cystoadenoma. Coronal T2-weighted image (a) shows a multiloculated, polylobate microcystic formation between the head, isthmus and hooked process process, characterised by areas of cribriform appearance and thin septa. MRCP image with MIP reconstruction (b) better shows the details of the morphology and fluid signal characteristics, the main duct has a regular course and calibre. In axial T1-weighted image with fat signal suppression after administration of intravenous contrast medium (c), the septa show contrast-graphic enhancement and centrally there is a hypointense area corresponding to fibro-sclerotic components.
Fig 1: Serous Cystoadenoma. Coronal T2-weighted image (a) shows a multiloculated, polylobate microcystic formation between the head, isthmus and hooked process process, characterised by areas of cribriform appearance and thin septa. MRCP image with MIP reconstruction (b) better shows the details of the morphology and fluid signal characteristics, the main duct has a regular course and calibre. In axial T1-weighted image with fat signal suppression after administration of intravenous contrast medium (c), the septa show contrast-graphic enhancement and centrally there is a hypointense area corresponding to fibro-sclerotic components.
2. Mucinous Cystic Neoplasms (MCNs)
- Almost exclusively affects women (>95%), average age ~45 years (‘mother lesion’)
- Primarily affects the distal pancreas
- WHO classification: MCN with low-grade dysplasia (adenoma), MCN with high-grade dysplasia (carcinoma in situ), MCN with invasive carcinoma
- Macroscopic presentation: multilocular macrocysts (most common); unilocular macrocysts, mimicking serous cystadenoma or pseudocyst
- MRI features: round cystic mass with sharp margins, parietal septa or nodules; capsular calcifications, thickened wall with contrast enhancement; mucinous content appears hyperintense on long TE sequences
- Management: due to malignant potential, MCNs should be excised when feasible
 Fig 2: Mucinous Cystoadenoma. Coronal (a) and axial (b) T2-weighted images show on the tail of the pancreas, a uniloculated cyst formation with thickened walls, in the absence of septal thickening or parietal nodules, with homogeneous fluid content, close to the main pancreatic duct, regular throughout its course, without being in communication with it. Axial T1-weighted image with fat signal suppression after administration of intravenous contrast medium (c) shows contrastographic enhancement of the walls.
Fig 2: Mucinous Cystoadenoma. Coronal (a) and axial (b) T2-weighted images show on the tail of the pancreas, a uniloculated cyst formation with thickened walls, in the absence of septal thickening or parietal nodules, with homogeneous fluid content, close to the main pancreatic duct, regular throughout its course, without being in communication with it. Axial T1-weighted image with fat signal suppression after administration of intravenous contrast medium (c) shows contrastographic enhancement of the walls.
3. Intraductal Papillary Mucinous Neoplasm (IPMN)
- Most common PCN (~70%)
- Usually affects elderly patients
- Classification: Main duct (MD) IPMN: segmental/diffuse main duct dilatation (>5 mm); Branch duct (BD) IPMN: Unifocal/multifocal cysts communicating with the mainduct; Mixed-type IPMN: Combined features of MD and BD-IPMN
- MRI features: communication with the pancreatic duct (best assessed by MRCP); parenchymal atrophy and altered pancreatic juice flow in MD-IPMN
- High-risk stigmata (HRS) (2023 Latest Kyoto Guidelines): jaundice, intramural nodules ≥5 mm with contrast enhancement, main pancreatic duct dilatation >10 mm
- Management: detailed imaging assessment with MRI and endoscopic ultrasound (EUS); EUS-guided fine-needle aspiration (FNA) for cytological analysis may provide additional diagnostic value; the presence of one or more HRS should prompt surgical consultation for possible resection.
 Fig 3: IPMN branch duct. MRCP coronal image with MIP reconstruction shows a voluminous multiloculated cyst formation on the hooked process that appears to be in communication with the main pancreatic duct, which is of regular calibre.
Fig 3: IPMN branch duct. MRCP coronal image with MIP reconstruction shows a voluminous multiloculated cyst formation on the hooked process that appears to be in communication with the main pancreatic duct, which is of regular calibre. Fig 4: IPMN main duct with signs of malignant degeneration. Coronal MRCP image with MIP reconstruction (a) shows marked and irregular dilatation of the main pancreatic duct with gradual increase in calibre. Axial T1-weighted image with fat signal suppression after administration of intravenous contrast medium (b) shows papillary proliferations in the main pancreatic duct at the level of the tail with discrete contrastographic enhancement.
Fig 4: IPMN main duct with signs of malignant degeneration. Coronal MRCP image with MIP reconstruction (a) shows marked and irregular dilatation of the main pancreatic duct with gradual increase in calibre. Axial T1-weighted image with fat signal suppression after administration of intravenous contrast medium (b) shows papillary proliferations in the main pancreatic duct at the level of the tail with discrete contrastographic enhancement.
Uncommon PCNs
4. Pseudopapillary Tumor
- Rare PCN with low malignant potential
- Typically affects young women (~35 years, ‘daughter lesion’)
- Commonly located in the pancreatic tail
- MRI features: well-encapsulated mass with mixed solid and cystic components; haemorrhagic necrosis contributes to cystic appearance; peripheral solid component enhances with contrast; haemorrhage appears hyperintense on short TE sequences
 Fig 5: Pseudopapillary Tumor. Axial T2-weighted image with fat signal suppression (a) shows at the head of the pancreas a polylobate-edged formation with inhomogeneous predominantly solid structure. Axial T1-weighted images (b) show an area of hyperintensity at the posterior site due to the presence of hemorrhage; after administration of intravenous contrast medium (c), contrastographic enhancement of the solid components is evident.
Fig 5: Pseudopapillary Tumor. Axial T2-weighted image with fat signal suppression (a) shows at the head of the pancreas a polylobate-edged formation with inhomogeneous predominantly solid structure. Axial T1-weighted images (b) show an area of hyperintensity at the posterior site due to the presence of hemorrhage; after administration of intravenous contrast medium (c), contrastographic enhancement of the solid components is evident.
5. Acinar Cell Carcinoma (ACC)
- Rare malignant tumor (~1-2% of pancreatic neoplasms)
- Occurs in males, peak incidence in childhood (8-15 years) and at ~60 years
- Most frequently in the pancreatic head
- MRI features: well-defined, round mass with cystic components; possible calcifications, necrosis, and hemorrhage; heterogeneous contrast enhancement
 Fig 6: Acinar cell carcinoma. Axial T1-weighted image with fat signal suppression after administration of intravenous contrast medium (a) shows on the hooked process of the pancreas a parenchymal formation with a mixed structure: a cystic posterior part with a solid token inside with contrast-enhancement and a solid anterior part. Coronal MRCP image with MIP reconstruction (b) shows the main pancreatic duct of regular calibre with evidence of accessory duct for the hooked process. Axial diffusion-weighted image (DWI) (c) shows signs of signal restriction of the solid components, presence of multiple sub-centimetric lymph nodes in the peripancreatic stations.
Fig 6: Acinar cell carcinoma. Axial T1-weighted image with fat signal suppression after administration of intravenous contrast medium (a) shows on the hooked process of the pancreas a parenchymal formation with a mixed structure: a cystic posterior part with a solid token inside with contrast-enhancement and a solid anterior part. Coronal MRCP image with MIP reconstruction (b) shows the main pancreatic duct of regular calibre with evidence of accessory duct for the hooked process. Axial diffusion-weighted image (DWI) (c) shows signs of signal restriction of the solid components, presence of multiple sub-centimetric lymph nodes in the peripancreatic stations.
6. Cystic Pancreatic Neuroendocrine Tumors (CPNET)
- Well-differentiated neuroendocrine tumors with a cystic component
- More frequent in patients with MEN1 syndrome
- Typically non-functional, occurring in adults (~50 years), predominantly in men
- MRI features: cystic lesion with well-vascularized tissue rim; arterial-phase enhancement with contrast; cystic component: low signal on short TE, high signal on long TE sequences
 Fig 7: Cystic NET with liver metastasis. Axial T2-weighted image (a) shows cystic lesion of inhomogeneous appearance in the tail of the pancreas with irregular thickening of the wall. Axial T1-weighted images with fat signal suppression after administration of intravenous contrast medium (b) in the early phase show early contrast-graphic enhancement of the wall and the presence (c) of a few millimetric focalities in the liver parenchyma with similar early contrast-graphic enhancement (one in particular with hyperintense border).
Fig 7: Cystic NET with liver metastasis. Axial T2-weighted image (a) shows cystic lesion of inhomogeneous appearance in the tail of the pancreas with irregular thickening of the wall. Axial T1-weighted images with fat signal suppression after administration of intravenous contrast medium (b) in the early phase show early contrast-graphic enhancement of the wall and the presence (c) of a few millimetric focalities in the liver parenchyma with similar early contrast-graphic enhancement (one in particular with hyperintense border).