
IMAGING
- Multi-Detector Computed Tomography (MDCT) with angiographic reconstructions (computed tomography angiography, CTA) is the gold-standard imaging technique for diagnosis and treatment planning. CTA should be performed in both arterial and venous phases since some pseudoaneurysms with a narrow neck are better visualised in the venous phase. Subsequent processing with Maximum Intensity Projection (MIP) and volume rendering reconstruction (VRT) can aid in visualisation and more accurately determine the location and origin of the pseudoaneurysm.
- Ultrasound (US) plays a less prominent role and is usable in the case of large pseudoaneurysms, or it can also be employed during the percutaneous approach in treatment. Its primary limitations are the presence of intestinal meteorism, patient constitution, and the deep location of the eHAPA. The main finding is represented by the presence of a hypoechoic lesion with a characteristic 'yin-yang' pattern on colour Doppler imaging.
- Magnetic Resonance Angiography (MRA) has a very limited role due to relatively long acquisition times, high cost, and low spatial resolution.
- Digital Subtraction Angiography (DSA) is the technique used to confirm the diagnosis and treatment in case of an endovascular approach [1, 2].
EMBOLIC AGENTS
Multiple agents can be used in the endovascular treatment of eHAPAs. These include stents, coils, liquid embolizing agents (e.g. glue or thrombin) and vascular plugs.
- Vascular stents are small tubular scaffolds widely used in the treatment of various circulatory disorders. They can be fabricated using different alloys (e.g. nitinol, stainless steel...), and can be bare or covered (e.g. PTFE). Deployment of a stent requires a distal and proximal neck and is limited by navigability in tortuous vessels. Flow-diverting stents can divert blood flow and determine a progressive thrombosis of the sac; they can maintain collateral vessel patency but are not recommended for eHAPAs.
- Coils and microcoils are embolising agents made of steel or platinum, available in different sizes and shapes and releasable in various ways (pushable, injectable or detachable). Their mechanism of action involves immediate mechanical blockage of blood flow and subsequent thrombosis. The diameter of the coils must be overestimated usually by 20-30%.
- N-butyl cyanoacrylate (glue) is a liquid embolising agent that polymerises on contact with anions: it is administered in a mixture with ethiodized oil, which acts as a solvent at various dilutions. The use of glucose solution after administration of the mixture prevents polymerisation of the glue within the administration instrument (needle in the percutaneous technique or microcatheter in the endovascular). The main complications are represented by non-target embolisation, catheter trapping and fragmentation.
- Lyophilized thrombin, derived from human plasma and mixed with calcium chloride solution before use, activates the coagulation cascade, leading to fibrin clot formation. Primarily used for percutaneous embolization, precautions include preventing reflux with endovascular balloon occlusion. Thrombin is contraindicated in cases of allergy or local infection, and complications such as non-target embolization, allergies, infections, and recurrence due to collateral supply or high flow are common issues.
- Vascular plugs (VPs) are a nitinol mesh occlusive device attached to a delivery system via a screw. Deployment involves unscrewing after positioning, and plugs should be oversized by 30–50% compared to vessel calibre. VPs offer better controlled deployment and high success rates. Although expensive compared to coils, it may be cost-effective in cases requiring multiple coils.
Each one of these materials or a combination of them allows different embolisation techniques [1, 2].
PRINCIPAL EMBOLISATION TECHNIQUES
There are several endovascular techniques used for treating eHAPAs
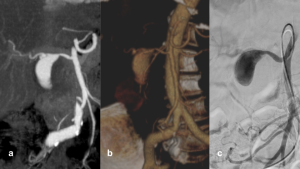
- Covered stent deployment (stent-graft)
Covered stent deployment (stent-graft) is one of the primarily used in our centre (fig.2, fig.3). It allows for the exclusion of the aneurysm while preserving blood flow to distal arterial branches. This technique is preferred in case of large neck eHAPAs and the limitations of this technique are essentially related to the presence of unfavourable anatomy. 

- Packing Embolization
In packing embolization the pseudoaneurysm sac is packed with coils, liquid embolic agents or particles (fig.4, fig.5). When coils are used, it can be a “stent assisted” technique and in this case, coils are released through the meshes of an uncovered stent (jailing), preventing migration and maintaining hepatic artery patency. The main limitation of this technique is limiting the visualisation in follow up CT due to the presence of hyperdense material. 

- Isolation embolization (Sandwich technique)
The isolation embolization technique involves excluding the inflow and outflow of the pseudoaneurysm using coils or plugs: it is a less commonly employed method due to the presence of collateral vessels (fig.6). This technique sacrifices the patency of the treated artery segment. It enables a more accurate assessment of vascular patency on follow-up CT scans. 
- Percutaneous combined approach
In complex cases, a combined endovascular and percutaneous approach with direct embolization of the pseudoaneurysmal sac with liquid embolic agents is also possible. In this technique, direct percutaneous ultrasound-guided puncture of the pseudoaneurysm is performed through a 21G Chiba needle (fig.7, fig 8). Then a mixture of N-butyl cyanoacrylate (glue) and ethiodized oil (low dilutions, 1:1,5) is slowly injected under fluoroscopic guidance in order to avoid reflux. When the pseudoaneurysmal sac is filled with the mixture, the Chiba needle is removed. Lyophilized thrombin can be used as an alternative embolizing agent [1, 5, 6]. 

FOLLOW-UP
Standardised follow-up protocol post treatment remains undefined; a reasonable approach involves imaging at peri-procedural, 3-month, 12-month, and subsequent yearly follow-up imaging. Early follow-up within the initial four weeks should prioritise assessing complete aneurysm occlusion and organ perfusion.
CTA is the preferred imaging modality, although artefacts may limit its use, prompting consideration of MRA or US depending on the endovascular treatment employed [1].
COMPLICATIONS
Main complications of treatment of eHAPAs are endovascular complications such as pseudoaneurysm rupture, arterial dissection, the ineffectiveness of embolizing treatment (endoleak, stent stenosis or stent occlusion, in case of covered stents), off-target migration of embolizing material and end-organ ischemia.
Secondary endovascular interventions may be required for reperfusion issues, depending on the cause such as additional coil packing for packing technique, new stent deployment or percutaneous embolisation for endoleaks in stent-grafting (fig. 8- 11). 



Other complications are arterial access site complications (hematoma, pseudoaneurysm...) and post-embolization (infection, abscess formation, post-embolization syndrome) [1, 2].