Hypoxic ischemic encephalopathy consists of a spectrum of brain abnormalities happening in the scenario of perinatal asphyxia
HIE is one of the leading causes resulting in cerebral palsy and other severe neurological deficits in children.
Conventional MRI identifies hypoxic brain injury after 24 hours, particularly after day 4. Novel MRI imaging modalities like diffusion-weighted imaging allow for faster diagnosis by relying on the restriction of diffusion in abnormal areas. DWI pseudo normalizes after about 7 days, during which conventional MRI is particularly helpful.
The APGAR score is a clinical tool used for evaluating neonates immediately after birth and in response to resuscitation. It comprises five factors: appearance, pulse, grimace, activity, and respiration. The APGAR score provides prognostic information regarding neonatal survival.
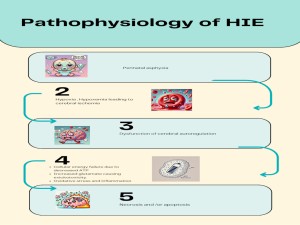
The pathophysiology of HIE starts with perinatal asphyxia leading to hypoxia and hypoxemia. There is consequent cerebral ischemia and loss of cerebral autoregulation. This culminates in a cascade of cellular events from cellular energy failure as a result of decreased ATP , Increased glutamate excitotoxicity , oxidative stress and inflammation , ultimately leading to necrosis and or apoptosis of brain cells
Different patterns of brain injury can be seen as part of HIE spectrum depending on the maturity of brain at time of insult , duration of ischemia and time for which the event has occurred . Four main patterns of injury can be seen.
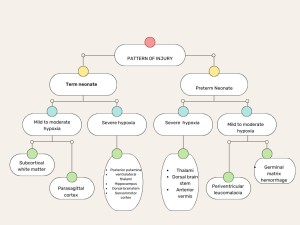
In preterm neonates a mild – moderate hypoxia can either affect the germinal matrix or lead to periventricular lecuomalacia.
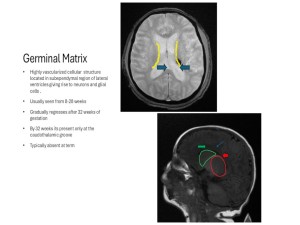
The germinal matrix hemorrhage can be graded into 4 types.
- Grade 1 : Subependymal matrix / germinal matrix (caudothalamic groove )hemorrhage
- Grade 2 : Grade 1 with extension of bleed into ventricles (<50%)
- Grade 3 : Grade 2 with extension into ventricles > 50% with ventricular dilatation
- Grade 4 : Any hemorrhage grade with involvement of brain parenchyma.
 Fig 4: Axial T2 propeller and SWI images of brain at the level of body of lateral ventricles showing subependymal grade 1 germinal matrix hemorrhage ( blue arrows )
Fig 4: Axial T2 propeller and SWI images of brain at the level of body of lateral ventricles showing subependymal grade 1 germinal matrix hemorrhage ( blue arrows ) Fig 5: Grade 4 germinal matrix hemorrhage ; Images a-d shows axial SWI images of a 36 weeks old neonate on 3rd day of life . Focus of blooming noted in right subependymal region extending to right lateral ventricle . Images e and f are axial T1 weighted images confirming the presence of hemorrhage with layering of hemorrhage in occipital horns of bilateral lateral ventricles . Image g shows the axial diffusion weighted imaging showing diffusion restriction involving right frontal region –likely PVHI.
Fig 5: Grade 4 germinal matrix hemorrhage ; Images a-d shows axial SWI images of a 36 weeks old neonate on 3rd day of life . Focus of blooming noted in right subependymal region extending to right lateral ventricle . Images e and f are axial T1 weighted images confirming the presence of hemorrhage with layering of hemorrhage in occipital horns of bilateral lateral ventricles . Image g shows the axial diffusion weighted imaging showing diffusion restriction involving right frontal region –likely PVHI. - Another pattern of injury which can be noted is periventricular leucomalacia . Its primarily due to the increased vulnerability of pre oligodendocytes to hypoxic stress. In acute phases it can be seen as areas of diffusion restriction involving periventricular white matter . It can also involve PLIC , corpus callosum and corona radiata.
 Fig 6: Image a and b are diffusion weighted imaging and ADC map of a 35 weeks old neonate on 4th day post natally at the level of basal ganglia . There is diffusion restriction involving splenium of cc , posterior periventricular white matter with extension upto cortex
Fig 6: Image a and b are diffusion weighted imaging and ADC map of a 35 weeks old neonate on 4th day post natally at the level of basal ganglia . There is diffusion restriction involving splenium of cc , posterior periventricular white matter with extension upto cortex -
Later it leads to paucity of periventricular white matter , cysts and irregularity of border and ex vacuo dilatation of lateral ventricles. In our study , no such cases were noted in the study population , likely secondary to the age group included .
In term neonates a mild to moderate hypoxia predominantly affects the watershed region of the brain with retained blood flow to the grey matter structures. This affects the parasagittal cortex and subcortical white matter .
 Fig 7: Mild-moderate pattern of HIE in a 5 day old term neonate . Diffusion restriction noted involving the parasagittal cortex and subcortical white matter with sparing of brain stem , cerebellum and deep grey matter .There is loss of normal T1 hyperintensity in PLIC
Fig 7: Mild-moderate pattern of HIE in a 5 day old term neonate . Diffusion restriction noted involving the parasagittal cortex and subcortical white matter with sparing of brain stem , cerebellum and deep grey matter .There is loss of normal T1 hyperintensity in PLIC -
If the hypoxia is profound , the blood flow to grey matter structures are also affected damaging posterior putamina , ventrolateral thalami , hippocampus , dorsal brain stem , sensorimotor cortex .
 Fig 8: Images a and b are axial diffusion weigted images of a 5 day old term neonate showing abnormal diffusion hyperintensity involving perirolandic region , corticospinal tracts , PLIC ventrolateral thalami and posterior putamina with the corresponding areas showing signal drop on ADC ( c , d ) . Loss of normal PLIC hyperintensity also noted ( f ) . Images e and f are axial T2 FLAIR and T1 weighted sequences at level of basal ganglia respectively . Apart from the loss of normal PLIC hyperintensity no other significant signal abnormality is noted involving same .
Fig 8: Images a and b are axial diffusion weigted images of a 5 day old term neonate showing abnormal diffusion hyperintensity involving perirolandic region , corticospinal tracts , PLIC ventrolateral thalami and posterior putamina with the corresponding areas showing signal drop on ADC ( c , d ) . Loss of normal PLIC hyperintensity also noted ( f ) . Images e and f are axial T2 FLAIR and T1 weighted sequences at level of basal ganglia respectively . Apart from the loss of normal PLIC hyperintensity no other significant signal abnormality is noted involving same . -
METHODS:
- Design: Cross-sectional study.
- Ethical Approval: Institutional Ethics Committee.
- Study Period: November 2022 to May 2024.
- Setting: Department of Radiodiagnosis, St. John’s Medical College, Bangalore.
Participants:
- Inclusion Criteria: Neonates (0-28 days) with provisional HIE diagnosis based on neurological symptoms (e.g., seizures, hypotonia, coma) and multiorgan dysfunction.
- Exclusion Criteria: Major congenital malformations, infections, metabolic diseases, MRI contraindications (e.g., pacemakers).
Sample Size:
- 35 neonates based on Syed et al., with a 90% detection rate and 10% precision at a 95% confidence interval.
MRI Protocol:
- Equipment: 3 Tesla GE MRI machine.
- Sequences: T2W, T1W, FLAIR, DWI, SWI.
 Fig 9: Utility of T1 weighted sequence in HIE.
Fig 9: Utility of T1 weighted sequence in HIE. Fig 10: Utility of T2 weighted sequence in HIE.
Fig 10: Utility of T2 weighted sequence in HIE. Fig 11: Utility of DWI sequence in HIE
Fig 11: Utility of DWI sequence in HIE Fig 12: Utility of SWI sequence in HIE
Fig 12: Utility of SWI sequence in HIE
-
- Imaging Duration: 52 seconds to 4 minutes 32 seconds.
- Analysis: Conducted by a postgraduate and a consultant radiologist.
Statistical Analysis:
- Software: SPSS.
- Techniques: Descriptive statistics, Pearson chi-square tests (P < 0.05).