- Imaging algorithm and follow-up
- MRI Features of Radiation-Induced Changes
- MRI Findings in Recurrent Cervical Cancer
- Advanced imaging techniques
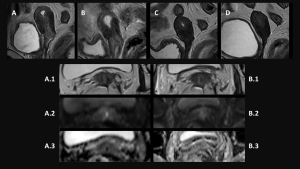
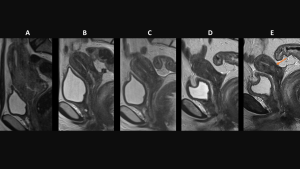
In patients with LACC a pre-treatment MRI is performed for loco-regional staging. Choosing proper sequences and correct plane angles is extremely important to avoid pitfalls in follow-up evaluation post-CRT. (Ciulla et al., 2022)
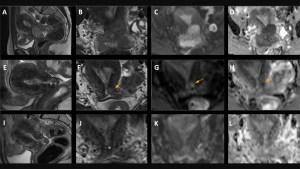
All subjects underwent 3Tesla MRIs, with T2-weighted imaging (oriented on cervical axial and coronal planes), diffusion-weighted imaging (DWI) (oriented on cervical axial plane) and dynamic contrast enhancement (DCE). The used protocol provides high anatomic resolution and is acquired on the cervical axis to provide better locoregional staging.
On MRI, the tumor presents an intermediate signal intensity on T2WI, a high signal intensity on DWI at high B-value and a low signal intensity on the apparent diffusion coefficient (ADC) map.
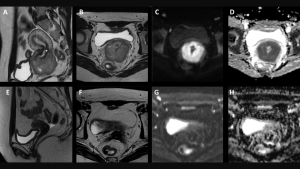
Accurate evaluation of tumor regression after therapy can be used to optimize therapeutic strategy and surgical procedure; MRI is the most reliable imaging modality for patients with LACC due to its high tissue resolution in the pelvis. Tumors treated with chemoradiotherapy (CRT) respond with a decrease in size and signal intensity on MRI. The response may be immediate (3–6 months) or, in larger tumors, delayed (6–9 months) (Manganaro et al., 2021)
Post-treatment MRI and FDG-PET/CT are usually performed at 3–6 months following CRT completion. Reconstitution of low-SI cervical stroma on T2WI indicates complete response; however, increased SI from CRT induced oedema, inflammation and necrosis may persist for up to 6 months, mimicking residual tumour.
2.1 Tumor Response:
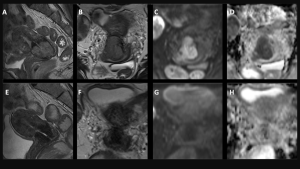
Radiation therapy typically leads to a reduction in tumor size, visible as early as 2 months post-treatment. MRI is essential for monitoring this decrease, which is often associated with a favorable prognosis. The primary tumor undergoes fibrotic changes, becoming contracted and displaying lower signal intensity on MRI.
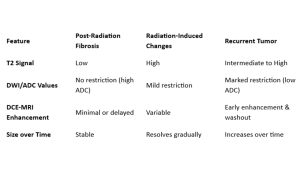
2.2 Post-radiation fibrosis occurs due to tissue scarring and loss of vascularity following radiation exposure. On MRI, fibrosis appears as low signal intensity on T2-weighted imaging, with well-defined borders and a lack of mass effect. It does not exhibit restricted diffusion on DWI and shows minimal or delayed enhancement on DCE-MRI, reflecting reduced vascularity (Lee et al., 2020). Fibrosis is often stable over time and does not increase in size, distinguishing it from progressive malignancy.
2.3 Fibrotic Changes in Adjacent Tissues:
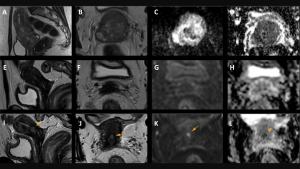
Following radiotherapy, adjacent pelvic organs and soft tissues often show fibrotic changes. These areas become hypointense, which may make them difficult to distinguish from the tumor, particularly during the first 6 months post-treatment. This fibrotic appearance can mimic tumor extension or parametrial invasion. In cases of advanced cervical cancer with initial parametrial invasion, contrast-enhanced MRI can help differentiate between radiation-induced fibrosis and residual or recurrent disease. PET/CT also plays a key role in this differentiation
2.4 Edematous Changes:
Edema is commonly seen in the bladder, rectum, sigmoid colon, and pelvic bowel loops after radiotherapy. In the bladder, a lobulated thickened T2-hyperintense area in the posterior bladder may be observed, with the T2-hypointense muscle layer preserved, suggesting bulbous edema rather than tumor tissue. Tumor invasion would show a loss of the T2-hypointense muscle layer with a similar tissue signal to the tumor on T2 imaging.
The accuracy of MRI depends on the time elapsed since the end of CRT. In the first six months after CRT, inflammation and edema contribute to a higher signal intensity on T2WI, which makes the diagnosis of locoregional residual disease more difficult.(van Kol et al., 2024)
Unlike fibrosis, radiation-induced edema is more transient and tends to resolve over weeks to months (Hricak et al., 2019).
These imaging features are crucial for differentiating between radiation-induced changes and residual/recurrent disease, and careful evaluation of the timing and characteristics of these findings is essential for accurate assessment.
2.5 Importance of DWI
The recent published ESUR guidelines (2021) for CC provide a central role of DWI sequences which are strictly recommended combined to T2-WI for a correct staging of CC and evaluation recurrence and response after therapy. (Manganaro et al., 2021)
Traditionally, Diffusion-Weighted Imaging (DWI) provides a qualitative assessment of malignant tumors with high cellular density. Therefore, the residual disease appears as an area of high signal, especially to high b-value, associated with lower ADC values compared to normal cervical stroma. DWI allows to distinguish the residual tumor from fibrosis, especially in the patients treated with radiotherapy, which on the contrary, presents low signal intensity at high b values and low signal intensity in ADC maps.
A recent multicenter prospective study found that DWI significantly increases the specificity of MRI in detecting local residual tumor compared to T2W imaging alone when assessing cervical cancer response after radiotherapy. (Ciulla et al., 2022)
Radiotherapy-induced fibrosis usually demonstrates low signal intensity on all sequences. However, in some cases, the signal intensity may be atypical and therefore it can be difficult to differentiate fibrosis from tumour. DWI is helpful in this scenario, as fibrosis does not demonstrate restricted diffusion. Post-contrast imaging is less useful as both fibrosis and tumour can demonstrate enhancement. (Shakur et al., 2023)

2.6 DCE-MRI
Regarding DCE-MRI, several studies found that poorly perfused presumably hypoxic tumors (low enhancement) had worse response to CRT, decreased locoregional control and reduced survival. There is no consensus on how to best analyse DCE-MRI and the standardization of the acquisition parameters and analysis remains a challenge. A recent study looking at the role of post-treatment DCE-MRI found that early avid enhancement of irradiated tumour compared to the myometrium was as a useful indicator of incomplete response; however, highly variable timing of post-treatment MRI limits conclusions. In light of these, the use of DCE-MR is considered optional with primary role lim ited to the research setting (Manganaro et al., 2021)

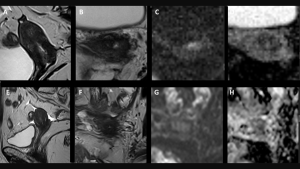
Recurrent cervical cancer often appears as a nodular or irregular mass with intermediate-to-high signal intensity on T2-weighted imaging and diffusion restriction on DWI. On DCE-MRI, recurrence exhibits early enhancement and washout, reflecting increased vascularity and metabolic activity (Huang et al., 2022). Compared to fibrosis, recurrent tumors demonstrate lower apparent diffusion coefficient (ADC) values, indicating increased cellular density (Lakhman et al., 2021). Additionally, PET-MRI can improve detection of metabolically active recurrent disease by combining anatomical and functional imaging data.
Emerging imaging techniques are improving post-treatment surveillance in cervical cancer. Radiomics extracts quantitative imaging biomarkers to differentiate benign from malignant changes with greater accuracy (Xu et al., 2023). PET-MRI integrates metabolic and anatomical imaging to detect viable tumor cells with higher sensitivity than MRI alone. MR spectroscopy further characterizes tissue composition by analyzing metabolic profiles (Kim et al., 2022). These advancements enhance diagnostic confidence and reduce the need for invasive procedures.