Alcohol
It is the most widely consumed legal drug worldwide. The mechanisms by which it causes damage to the central nervous system (CNS) may include direct ethanol toxicity or indirect effects, such as the presence of contaminants in alcoholic beverages or diseases affecting other organs (e.g., liver disease) that impact the CNS.
- In acute intoxication, structural alterations in the CNS are generally not observed.
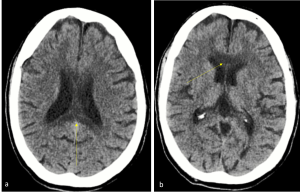
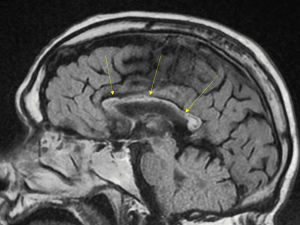
- Wernicke's Encephalopathy: Caused by thiamine (vitamin B1) deficiency; therefore, it can also occur in non-alcoholic patients. Most commonly affected areas: mammillary bodies, medial thalamus, tectum, periaqueductal gray matter, and areas around the third ventricle.
CT findings: Nonspecific, hypodensity around the third ventricle.
MRI findings: T1- weighted hypointensity and ; T1- weighted + Gd may show enhancement, most frequently in the mammillary bodies; restricted diffusion can be observed in affected areas; MR spectroscopy: Decreased N-acetylaspartate (NAA) and elevated lactate peaks.



- Marchiafava-Bignami Disease: Occurs in chronic alcoholic patients and is attributed to a deficiency of all eight types of vitamin B, leading to demyelination and necrosis of the corpus callosum, primarily affecting the genu and splenium, which may eventually result in areas of atrophy.
CT findings: Hypodensity.
MRI findings: T1- weighted hypointensity, T2- weighted /FLAIR hyperintensity in the acute phase, while in the chronic phase, areas of hypointensity may appear; possible diffusion restriction; MR spectroscopy: Decreased NAA in the acute phase.
- Chronic Alcoholic Encephalopathy: Predominantly frontal and infratentorial atrophy
Cocaine
It is an alkaloid extracted from the leaves of the Erythroxylon coca plant and is the second most consumed illegal drug. There are two forms: freebase cocaine (crack), which is smoked, and cocaine hydrochloride, which is water-soluble and is well absorbed through mucous membranes. The most frequent complications occur when consuming cocaine hydrochloride (snorting).
- Ischemic lesions: These do not follow a vascular pattern and are more commonly found in border territories, although cases have been described both supratentorially and infratentorially. In angiographic MRI, the focal occlusion point can be identified due to arterial spasm and/or vasculitis, where peripheral vessel enhancement can also be observed after intravenous contrast administration.
- Cerebral hemorrhage: It can be intraparenchymal and/or subarachnoid, caused by a sustained increase in blood pressure, which increases the risk of rupture of pre-existing aneurysms and arteriovenous malformations. Intraparenchymal hemorrhage is much more frequent in the basal ganglia and thalami, which tend to rupture into ventricles more easily than in non-cocaine users.
 Fig 6: Axial CT shows an extensive acute subarachnoid hemorrhagic component in the sulci of both cerebral hemispheres, more voluminous in the left Sylvian fissure, as well as in the perimesencephalic cisterns. This was later confirmed on diagnostic angiography to correspond to a ruptured aneurysm of the left middle cerebral artery (no images are available due to an internal technical error).
Fig 6: Axial CT shows an extensive acute subarachnoid hemorrhagic component in the sulci of both cerebral hemispheres, more voluminous in the left Sylvian fissure, as well as in the perimesencephalic cisterns. This was later confirmed on diagnostic angiography to correspond to a ruptured aneurysm of the left middle cerebral artery (no images are available due to an internal technical error). - Mucosal and bone alterations: Snorting cocaine causes ischemic necrosis due to vasoconstriction, which can lead to nasal mucosal atrophy and septal perforation, visible on CT.
It has also been reported cases of reversible posterior leukoencephalopathy syndrome (PRES).
Heroin
Heroin is a synthetic opioid derived from morphine, and it can be consumed orally, intravenously, or by inhalation. Complications on the central nervous system (CNS) may arise from direct or indirect toxic effects (due to impurities, route of administration, etc.).
- Spongiform leukoencephalopathy: This is a complication following inhaled use, a technique known as "Chasing the Dragon" or "Chineseing." It affects the cerebellum, sparing the dentate nuclei. On MRI, it appears as areas of hyperintensity in T2/FLAIR in a "butterfly" pattern in the cerebellum, respecting the dentate nuclei, perirrolandic subcortical white matter, the posterior limb of the internal capsule, and the pontine corticospinal tracts. It may show diffusion restriction in the acute phase. Magnetic Resonance Spectroscopy (MRS) may show a decrease in N-acetylaspartate (NAA) and an increase in lactate. On CT, it appears as areas of hypodensity.
 Fig 7: a. Axial T2- weighted MRI image shows high-signal-intensity in a "butterfly" pattern in the cerebellum, respecting the dentate nuclei; in the CT (b) hypodensity is observed. c. Schematic image, with the dentate nuclei in orange and the white matter of the cerebellum in blue.
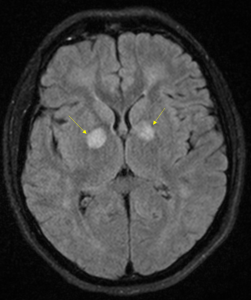
Fig 7: a. Axial T2- weighted MRI image shows high-signal-intensity in a "butterfly" pattern in the cerebellum, respecting the dentate nuclei; in the CT (b) hypodensity is observed. c. Schematic image, with the dentate nuclei in orange and the white matter of the cerebellum in blue. - Ischemic complications: Bilateral and symmetrical involvement of the globus pallidus; in the long term, it may lead to small vessel disease at earlier ages.
- Infectious complications: Abscesses or septic emboli to the CNS may occur following intravenous use.
Cannabis
Cannabis is derived from the dried flowers and leaves of the Cannabis sativa or Cannabis indica plants. There are several methods of preparation and consumption: marijuana, which can be smoked, vaporized, or incorporated into edibles, and hashish, which is typically smoked or vaporized. The primary psychoactive compound responsible for its effects is tetrahydrocannabinol (THC).
Imaging findings related to cannabis use are generally nonspecific. However, cannabis consumption has been associated with ischemic complications, primarily due to mechanisms such as vasospasm, vasculitis, or secondary hypotension. The most commonly affected structures are the basal ganglia, although both supra and infratentorially infarcts can occur, without following a typical vascular distribution.
In a perfusión MRI an increase in cerebral blood flow (CBF) may be observed in the acute phase, whereas in long-term abuse patients, a decrease in CBF is seen.
Amphetamines and Derivatives
Amphetamines produce a potent vasoconstrictive effect through the rapid release of biogenic amines, particularly MDMA, which acts by releasing serotonin (5-HT). Its receptors are predominantly distributed in the globus pallidus and occipital cortex, where infarcts tend to occur, often exhibiting bilateral and symmetrical involvement.
They can also lead to intracranial hemorrhage, especially in patients with preexisting aneurysms or arteriovenous malformations (AVMs), due to the sharp increase in blood pressure following consumption.
- Posterior reversible encephalopathy syndrome (PRES)—also known as acute hypertensive encephalopathy: affects the posterior circulation and cortical watershed areas, where hypertension is believed to cause endothelial damage and blood-brain barrier disruption, leading to vasogenic edema. This condition is also seen in users of other substances such as cocaine.
CT Scan: Findings may be subtle, showing non-confluent cortico-subcortical hypodensities that are bilateral and symmetrical, most frequently affecting the posterior parietal and occipital lobes.

MRI (More Sensitive for Diagnosis): T2/FLAIR: Shows hyperintensity in the parieto-occipital regions. However, there may also be bilateral and symmetrical involvement of the basal ganglia, brainstem, and cerebellum. Post-contrast T1-weighted MRI: May show patchy enhancement after intravenous contrast administration. Perfusion MRI: May demonstrate an increase in relative cerebral blood flow (rCBF). MRS can reveal increased choline and creatine levels.

Early MRI evaluation is crucial when PRES is suspected, as it allows for earlier detection of these alterations compared to CT.
In chronic users, atrophy is observed, which is variable but selectively affects the occipital lobes.