Out of 5,066 educators, a total of 373 valid responses were received, which yielded a response rate of 7.4%. The geographical distribution of the responses across the States can be seen below.

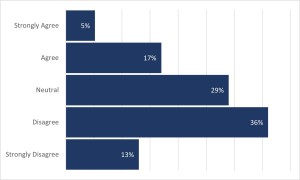
Respondents were also asked to indicate their level of agreement with the statement, ‘’I have appropriate training to learn and apply new technology, including AI/ML automation”. The responses are summarised below. A 22% of the respondents answered this question favourably (strongly agree and agree), while 49% answered the question unfavourably (strongly disagree and disagree).
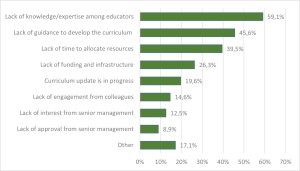
Most respondents stated that their educational programs (283/371, 76.3%) did not include AI in their curricula. Only a quarter (88/371, 23.7%) have integrated AI-related education into their programs. Respondents who indicated that their programs did not include education on AI were asked to report the main reasons for not including it in their curricula.
Patient positioning was the topic most commonly taught using AI-enabled tools (19/38, 50%), followed by image quality assessment (16/38, 42.1%), radiation physics (16/38, 42.1%), pathology (14/38, 36.8%), anatomy (13/38, 34.2%), radiographic anatomy (12/38, 31.6%), radiation protection (11/38, 28.9%), patient care (9/38, 23.7%), communication skills (6/38, 15.8%), and professionalism classes (4/38, 10.5%). Additionally, 13.2% (5/38) reported using AI-enabled tools for all aspects of teaching/learning.
When asked about the support they received from department leaders or management for implementing new processes or procedures related to new technologies such as AI/ML, many respondents (158/368, 42.9%) were neutral, indicating neither strong support nor lack of support. Roughly equal numbers felt they received appropriate support (88/368, 23.9%) as felt they did not receive sufficient support (82/368, 22.3%).
Slightly over half (198/362, 54.7%) of the respondents believed that MRT professionals will leave patient-centred clinical work in favour of working for technology companies developing AI tools, compared to those who did not believe this (164/362, 45.3%). The future of the profession is viewed to be more positive with the implementation of AI for many of the respondents (295/358, 82.4%).