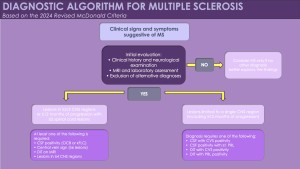
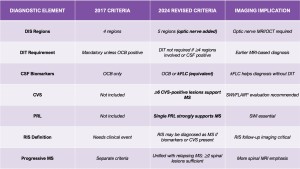
The McDonald criteria, first introduced in 2001, transformed MS diagnosis by formally incorporating MRI into the diagnostic process. Subsequent revisions in 2005, 2010, and 2017 refined this approach, emphasizing MRI and adding CSF oligoclonal bands as supportive markers, enabling earlier and more reliable diagnosis. Traditionally, MS diagnosis required demonstrating dissemination in space (DIS) and dissemination in time (DIT), representing separate demyelinating events across different CNS regions and time points.
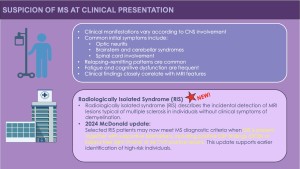
However, this long-standing model is now being reconsidered. The 2024 revision introduces a more biologically grounded diagnostic framework that integrates blood and CSF biomarkers, optic nerve assessment via MRI and OCT, and radiological markers such as the central vein sign (CVS) and paramagnetic rim lesions (PRLs). Importantly, the updated criteria also allow certain cases of radiologically isolated syndrome (RIS) to be classified as MS, marking a significant conceptual shift in the diagnostic landscape.
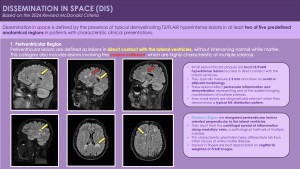
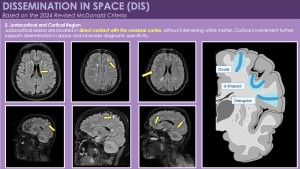
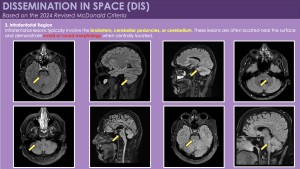
1. Dissemination in Space (DIS): Updated MRI Definition
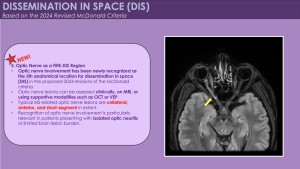
According to the 2024 McDonald criteria, dissemination in space is demonstrated by typical demyelinating lesions in at least two of five anatomical regions:
- Periventricular
- Juxtacortical / Cortical
- Infratentorial
- Spinal cord
- Optic nerve (newly included)
The inclusion of the optic nerve represents a major imaging update and supports earlier diagnosis, particularly in patients presenting with optic neuritis. Optic nerve involvement can be confirmed using orbital MRI, supported by OCT and visual evoked potentials (VEP) when required.

2. Dissemination in Time (DIT): Flexible Imaging Requirements
MRI-based evidence of DIT may still be demonstrated by:
- Simultaneous presence of gadolinium-enhancing and non-enhancing lesions on a single MRI
- Appearance of new T2 or enhancing lesions on follow-up imaging
However, under the 2024 criteria, DIT is no longer mandatory when robust biological or topographic evidence is present. This change reduces dependence on longitudinal imaging and allows earlier diagnosis.
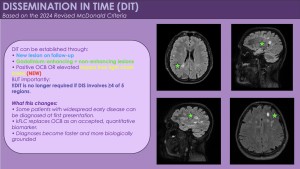
3. MRI-Only Diagnosis in Widespread Disease
In patients with typical clinical presentations, MS can be diagnosed based on imaging alone when:
- Lesions are present in ≥4 of the 5 DIS regions
In this scenario, neither DIT nor CSF biomarkers are required, provided that lesion morphology and distribution are characteristic of MS.
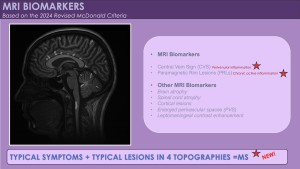
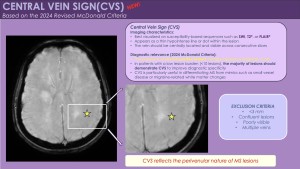
4. Central Vein Sign (CVS): Imaging Marker of Specificity
The central vein sign (CVS) is a radiological biomarker that increases diagnostic specificity for MS:
- Defined as a small vein running through the centre of a white matter lesion
- Best visualized on SWI, T2*, or FLAIR* sequences
- ≥6 CVS-positive lesions strongly support MS diagnosis
In patients with fewer than 10 white matter lesions, the majority of lesions should demonstrate CVS to maintain specificity.
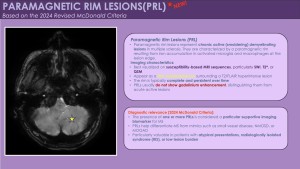
5. Paramagnetic Rim Lesions (PRLs): Chronic Active Lesions
PRLs represent chronically active demyelinating lesions characterised by:
- A hypointense rim on susceptibility-weighted imaging
- Iron-laden activated microglia at the lesion edge
- High specificity (>90%) for MS
The presence of even a single PRL provides strong diagnostic support, especially in challenging or atypical cases.
6. Imaging Criteria in Radiologically Isolated Syndrome (RIS)
Under the 2024 revision, RIS may fulfil diagnostic criteria for MS when imaging shows:
- DIS according to the 5-region definition and
- Supportive imaging or biological markers, such as: ≥6 CVS-positive lesions,positive CSF biomarkers (OCB or kFLC)
This represents a fundamental shift in the imaging-based interpretation of RIS.
7. Imaging in Progressive Multiple Sclerosis
The same imaging framework applies to both relapsing and progressive MS.For primary progressive MS (PPMS):
- ≥2 spinal cord T2-hyperintense lesions are sufficient to meet DIS
- This reflects the strong predilection of MS for spinal cord involvement in progressive disease
Spinal MRI, therefore, plays a critical role in this subgroup.
8. Recommended MRI Protocols
To reliably detect DIS, DIT, CVS, and PRLs, the following MRI sequences are recommended:
- 3D FLAIR
- T2-weighted imaging
- SWI or T2* for CVS and PRLs
- Post-contrast 3D T1-weighted imaging
- Thin-slice spinal cord MRI (≤3 mm)
Standardised protocols improve reproducibility and diagnostic confidence.