CFE is a serious, potentially lethal complication of orthopedic and other procedures or trauma that occurs after the release of fat emboli into the bloodstream. Brain involvement may be isolated or associated with respiratory and skin symptoms and signs that characterize fat embolism syndrome (FES)
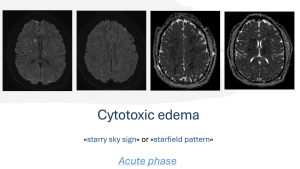
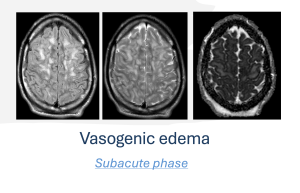
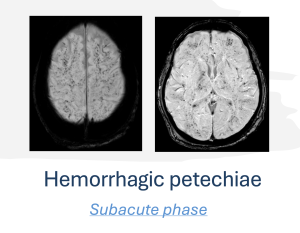
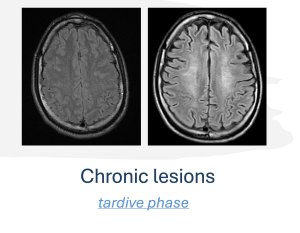
MRI of the brain is the fundamental diagnostic tool and there is a correlation between MRI findings, the severity of symptoms and developmental stages (acute, subacute, and chronic phases).
MRI patterns typically evolve in alignment with the progression of the disease. In the acute phase, cytotoxic edema is often observed, presenting as a "starry sky sign" or "starfield pattern”
We conducted a retrospective observational study, examining all cases of polytrauma treated in our hospital between 2017 and 2023, that were complicated by the onset of CFE (7 patients). The inclusion criteria were diagnosis of polytrauma and access to the emergency room for immediate treatment. All patients included in the study underwent the following diagnostic procedures:

Upon access to emergency department, all patients have undergone a trauma diagnostic imaging protocol, which includes:
- Computed tomography (CT) of the skull
- CT total body with a contrast agent
- CT angiography of epiaortic vessels
- Radiography (X-Ray) in case of a fracture of the upper or lower limbs
Following neurological deterioration, an urgent CT scan of the skull was performed without a contrast agent.
Clinical suspicion of CFE, according to the clinical criteria of Gurd et al., was confirmed by MRI of the brain without contrast medium.
We analyzed the findings from the CT scans of the skull and CT angiography of the epiaortic vessels, performed in urgency at the time of access to emergency department, as well as the presence of any bone fractures, dividing them into fractures of the upper limbs, lower limbs or both.
Subsequently we analyzed the findings of urgent CT required in case of neurological deterioration.
Finally, the findings from MRI examination were evaluated in order to assess whether they met the diagnostic criteria of CFE, and to analyze the distribution of restriction areas in diffusion-weighted imaging (DWI) and the possible mismatches between the DWI and Fluid-Attenuated Inversion Recovery (FLAIR) sequences.
All data obtained were compared to assess the correlation between radiological findings and clinical diagnosis, as well as to identify any specific diagnostic patterns.