MPCs are uncommon and predominantly benign, often referred to as “do not touch” lesions. These cysts arise from diverse anatomic structures and are sometimes associated with genitourinary abnormalities or symptoms.Although transrectal ultrasound and CT imaging play supportive roles, pelvic MRI remains the preferred diagnostic tool, providing noninvasive and detailed visualization of the prostate gland and associated structures.
MPCs can be categorized into two main groups: intraprostatic and extraprostatic cysts.
A-Intraprostatic cysts :
When considering the location, Intraprostatic cysts can be further classified into median cysts, paramedian cysts, and lateral cysts.
Median intraprostatic MPCs prompt the hypotheses of utricle or müllerian duct cysts.
Müllerian duct cysts : [1,2]
- Müllerian duct cysts arise from remnants of Müllerian ducts and are more commonly identified in the 3rd or 4th decade of life.
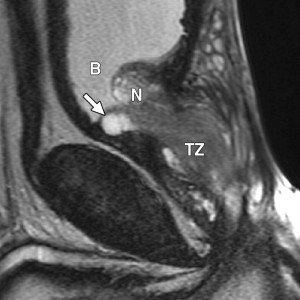
- They do not communicate with the urethra and may contain calculi. Typically tear-shaped, these cysts extend above the prostate and may deviate slightly from the midline.They contain sperm-free brownish fluid, which is of high signal intensity on T2-weighted images. Calculi may cause hemorrhage into the cyst, which can be demonstrated on T1-weighted images. Symptomatic cases can present with urinary retention, urinary tract infections, or ejaculatory duct obstruction. Carcinoma development, while rare, remains a potential complication.
- Although the current literature presents some debate over whether Müllerian duct cysts (MDCs) and prostatic utricle cysts (PUCs) are identical or represent separate entities,recent studies distinguish Müllerian duct cysts from utricle cysts based on immunohistochemical evidence, which shows distinct embryological origins.
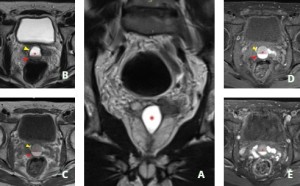
Prostatic Utricle Cysts [3]
- Typically diagnosed in childhood, Prostatic Utricle Cysts originate from the verumontanum and are always midline structures, measuring 8–10 mm in length.They are pear-shaped and do not extend beyond the base of the prostate, features that helps distinguish it from a mullerian duct cyst. Utricle cysts are often linked to conditions such as hypospadias, pseudohermaphroditism, and cryptorchidism.
-
Müllerian duct cysts and prostatic utricle cysts are susceptible to infection, often resulting in pus accumulation. This can complicate imaging interpretation, as their presentation may closely mimic that of prostatic abscesses or cystic tumors, leading to diagnostic uncertainty.
Paramedian intraprostatic MPCs are most associated with ejaculatory duct cysts or urethral diverticulum.
Ejaculatory duct cyst[4]
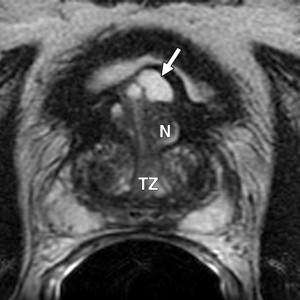
- Ejaculatory duct cyst lesions point to the seminal caruncle of the prostate and are associated with dilated ipsilateral seminal vesicles.
- They appear to be cystic structures along the ejaculatory duct just lateral to the midline in the central zone of the prostate. However, when they are large, they may extend cephalad to the prostate and appear to arise centrally.
- They are of high signal intensity on T2-weighted images, but commonly contain calculi that have low signal intensity.
- Laboratory examinations of the cystic fluid contain sperm, while the Müllerian duct cyst fluid does not contain sperm.

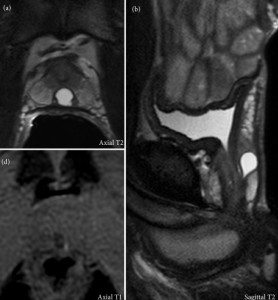
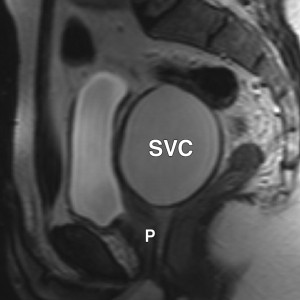
Urethral diverticulum [5]
- Urethral diverticulum (UD) is a rare condition characterized by saccular dilatation of the urethral wall, which can be congenital (10%) or acquired (90%).It has a peak age incidence of 25–45 years.
- UD MRI will show a periurethral abnormality that can be round, partially circumferential or "saddle-bag" in shape and communicates with the urethral lumen, allowing to make a definitive diagnosis.
Lateral intraprostatic MPCs include prostatic retention cysts, cystic degeneration of benign prostatic hypertrophy, abscesses, or tumors.
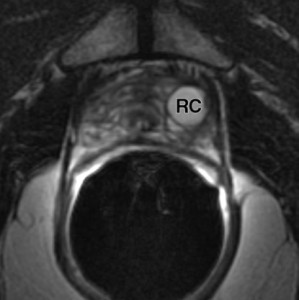
Prostatic retention cysts [6]
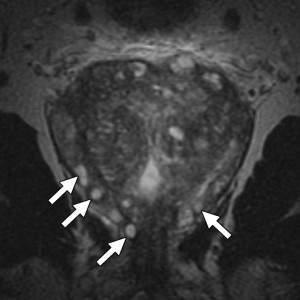
- Prostatic retention cysts typically develop in individuals in their 50s or 60s and are often asymptomatic. Commonly associated with benign prostatic hyperplasia (BPH), these cysts form due to dilatation of glandular acini caused by acquired ductal obstruction.
- They are characterized by smooth-walled,usually round cysts and can appear in any prostate zone. Diagnosis is based on their presence in the peripheral zone and the absence of other findings indicative of BPH.
Cystic degeneration of benign prostatic hyperplasia (BPH): [6]
- Cystic degeneration of BPH is a common lesion arising from degenerative changes in BPH within the transitional zone of the prostate.
- These cysts often exhibit irregular shapes and variable sizes, sometimes containing hemorrhagic material or calculi. Patients with such lesions typically experience urinary obstruction symptoms linked to BPH.
Prostatic abscesses [7]
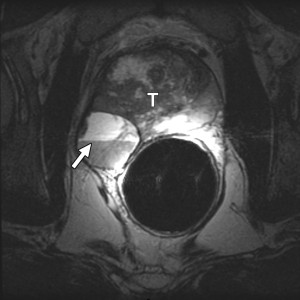
- Prostatic abscesses are rare and may present as cystic lesions in any part of the prostate. Diagnosis primarily relies on clinical evaluation.
- While MRI is not typically used for this condition, an abscess should be considered when imaging reveals a cystic lesion with thickened walls, septations, or heterogeneous content, in patients with characteristic clinical symptoms.
Cystic carcinoma[8]
- A cystic carcinoma should be suspected if the cyst grows rapidly or if it has irregular walls, irregular signal intensity, or a solid component.
B-Extraprostatic cysts :
Extraprostatic cysts include cysts of the seminal vesicle, vas deferens, and Cowper duct.
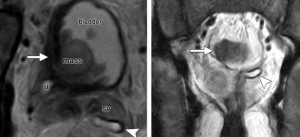
Seminal vesicle cysts :[9]
- Seminal vesicle cysts, which develop laterally, are caused by congenital atresia of the ejaculatory duct. These cysts are typically unilateral and often extend into the bladder. Their contents are frequently hemorrhagic and contain inactive spermatozoa.
Cysts of the Vas Deferens : [6]
- Cysts of the Vas Deferens are located superior to the prostate gland along the course of the vas deferens. On MRI,they are easily recognized and distinguished from other adjacent structures.
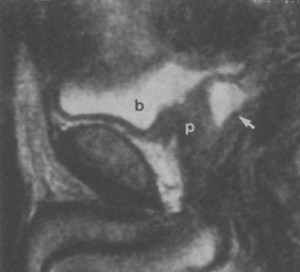
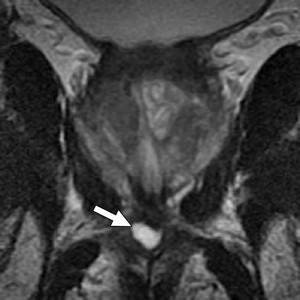
Cowper gland cysts :[6]
- The Cowper gland ducts drain into the bulbous urethra, and their obstruction may lead to the formation of retention cysts. While most Cowper duct cysts are asymptomatic, larger ones may cause hematuria, urinary obstruction, or even male infertility.
- Typically, they appear at MR imaging and transrectal US as a unilocular cystic lesion at the posterior or posterolateral aspect of the posterior urethra.
Most prostate cysts are benign and self-healing,surgical interventions especially minimally invasive treatments are recommended for symptomatic midline prostatic cysts and malignant prostatic cysts.