We present a series of cases, with a range of patient demographics, demonstrating suspicious radiological findings with subsequent histology results confirming alternative diagnoses which were benign.
These include:
- Benign urothelial tumour: Inverted papilloma
- Infectious cause: Schistosomiasis
- Inflammatory cause: Polypoid cystitis
- Iatrogenic cause: Radiation cystitis
On a retrospective review, we share learning points from each of these cases. We propose a mnemonic 'MIMIC' to categorise the underlying diagnoses.
Benign Mass - Inverted urothelial papilloma
Inverted Urothelia Papillomas (IUP) are rare, non invasive papillary lesions covered by urothelium, exhibiting an endophytic growth pattern. They can occur anywhere along the urinary tract, with 90% found in the bladder [1]. The clinical presentation, cystoscopy findings (pedunculated mass or polypoid/papillary tumour with a smooth surface), as well as imaging findings do not distinguish IUP from inverted growth pattern TCC.
Our case (Fig.1) demonstrates typical findings of IUP on CT urogram; a mass arising from the bladder wall. On MRI, IUP tends to be isointense on T1, iso/hyperintense on T2 (relative to the bladder wall) and demonstrates early contrast enhancement. These imaging features are also shared with urothelial carcinoma [2].
The peak age of incidence is the 5th and 6th decade however in our case, the patient is significantly younger (24 years old) indicating the broad patient demographic and diagnostic challenge.
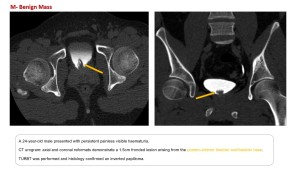
Treatment of lower urinary tract IUP involves transurethral resection. Although these are benign lesions there is an increased risk of concomitant or subsequent TCC hence patients will undergo regular follow up cystoscopies [2].
Infection - Schistosomiasis
Infection by the Schistosoma fluke is endemic in the developing world. This parastic infection is contracted by humans coming into direct contact with infected water containing parasitic larvae released from freshwater snails. These larvae reside and mature in the lungs and liver of the human host. After maturation, the parasite migrates along the vascular endothelium to the vesical venous plexus, situated at the fundus of the urinary bladder. Eggs are produced, inciting a localised granulomatous reaction. The eggs also migrate through the bladder wall to be shed in urine/faeces, hatch, infect the freshwater snails and continue to spread the infection [3].
In the acute phase, nodular or diffuse bladder wall thickening is seen on urography or cross sectional imaging [4].
In the chronic phase, the classic radiological finding is of bladder wall calcification secondary to the deposition of dead eggs in the submucosa. Over time, the bladder becomes fibrotic and contracted. Chronic irritation of the bladder can also result in cystitis glandularis; a disorder of glandular metaplasia and proliferation of the urothelium (transitional cells). In the late stage of this disorder, a papillary or polypoid mass of the bladder wall can be seen [3].
It is important to note that the extent of bladder wall calcification is correlated to the number/concentration of schistosome eggs [5]. Hence the lack of bladder wall calcification does not exclude the diagnoses of Schistosomiasis, as demonstrated in our case (Fig. 2) which shows other features of chronic infection.
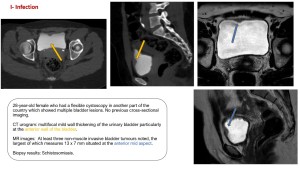
Schistosomiasis is a risk factor for the development of urinary bladder carcinoma, particularly squamous cell carcinoma [3].
InflaMmation-Polypoid cystitis
Polypoid cystitis is a benign exophytic lesion with the most well-known aetiology related to long term catheterisation, although there are cases in the literature unrelated to indwelling catherisation, as was the case with our patient [6], [7]. Chronic irritation of the bladder results in hyperplasia of the urothelium and the development of polypoid lesions of variable sizes [6]. In our case (Fig. 3), there is only a small filling defect at the bladder dome.
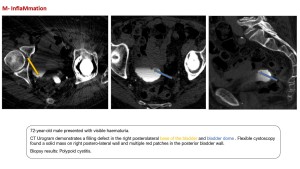
A key difference between polypoid cystitis and cystitis glandularis described in the previous case, is in the histological appearances, with polypoid cystitis featuring minimal metaplasia. Both of these conditions are non-muscle invasive unlike urothelial carcinoma [6].
Although benign and reversible, large masses can become obstructive and may require resection [6].
Iatrogenic- Radiation cystitis
Radiation cystitis is a potential complication following treatment of pelvic cancers. Despite advances in radiation technique with the delivery of targeted therapy, the bladder is sensitive to low doses of radiation [8]. The adverse effects are categorised as acute and chronic, with acute radiation cystitis occuring upto three months after the completion of radiation therapy. In the acute phase, the bladder mucosa is damaged, there is desquamation of the epithelium and haemorrhagic cystitis. On imaging, the bladder wall is focally or diffusely irregularly thickened. As well as inflammation, hyperaemia can result in bleeding with intraluminal clot seen on ultrasound or CT. MR imaging can be helpful to distinguish the bladder wall and clot [9].
Late radiation cystitis occurs a minimum of three months after cessation of radiation therapy. It can even be seen a few years later [8] as demonstrated in our case (Fig. 4), with the patient presenting four years after external beam radiation for prostate cancer. Cystoscopy also showed prominent blood vessels throughout the bladder typical of radiation cystitis changes.
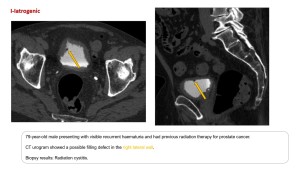
Other features include obliterative endarteritis of the submucosal vessels, ischaemia and fibrosis resulting in a small, fibrosed thick walled bladder and resultant hydronephrosis. Mucosal ulcers and fistulisation can also be seen [9].
Treatment is largely supportive. In refractory haematuria arterial embolisation or even cystectomy with urinary diversion may need to be performed [8],[9].