Spondylodiscitis most commonly affects the lumbar spine (58%), followed by the thoracic spine (30%) and cervical spine (12%). In 65% of patients, the infection is limited to a single vertebral level. In contrast 25% of patients experience involvement at multiple vertebral levels, with 10% of the cases demonstrating lesions at non-contiguos level.
Plain radiograph
Conventional radiography is often the primary method used in the initial assessment of patients presenting with back pain; however, it has limited sensitivity in detecting early changes. During the acute phase, radiographs typically appear normal. Thereafter signs such as decreased disc space height or endplate erosions may become apparent. Later manifestations, typically occuring during 8 to 12 weeks after the onset, include vertebral reactive sclerosis or collapse adjacent to a narrowed disc space. Overtime, gradual obliteration of the intervertebral disc can be detected, leading to the formation of a vertebral block. (Fig.3)

Computed tomography
CT can identify bony changes earlier than conventional radiography, although it may still appear normal during the first weeks of infection.The main imaging findings include:
- Disc space narrowing
Often the earliest manifestation of the disease, accompanied by decreased attenuation of the disc. Occasionally, gas in the disc space (vacuum phenomenon) can be observed.
- Bony destruction
Early stages may show subtle vertebral endplate erosions, while more advanced stages reveal significant bone destruction, loss of normal trabecular bone architecture, bony sclerosis and vertebral collapse of the vertebra. (Fig.4)
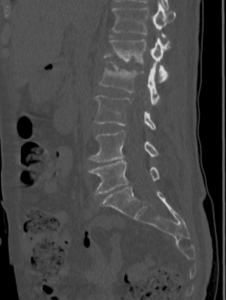
- Spinal deformity (scoliosis, kyphosis) (Fig.5)
 Fig 5: Coronal CT scan of the lumbar spine: bony destruction of the inferior endplate of L1 and the superior endplate of L2 including spinal deformity at this level
Fig 5: Coronal CT scan of the lumbar spine: bony destruction of the inferior endplate of L1 and the superior endplate of L2 including spinal deformity at this level - Paravertebral soft tissue involvement and abscess formation (Fig.6)
 Fig 6: Sagittal CT scan of the dorsal spine (soft tissue window): spondylodiscitis at the level T8-T9 with endplate erosions and formation of a paravertebral abscess at this level
Fig 6: Sagittal CT scan of the dorsal spine (soft tissue window): spondylodiscitis at the level T8-T9 with endplate erosions and formation of a paravertebral abscess at this level
Increased attenuation in the paraspinal region is indicative of inflammation. The formation of abscesses in the paravertebral region is a critical complication of spondylodiscitis. These abscesses appear as well-defined, hypoattenuating fluid collections. Contrast-enhanced CT scans provide better delineation, revealing peripheral enhancement, which indicates increased vascularity and inflammation associated with the infection.
In more advanced cases, the infection may extend beyond the paravertebral soft tissues into the epidural space, forming an epidural abscess that can cause compression of the spinal cord or nerve roots. (Fig. 7)

CT also offers advantages in guiding biopsy procedures and assessing post-treatment changes.
MRI
Is the gold standard for diagnosing spondylodiscitis due to its superior soft tissue contrast and ability to detect early inflammatory changes. The main imaging findings include:
- Early disc and vertebral involvement
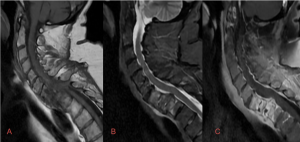
* hypointense on T1-weighted images, hyperintense on T2 images (inflammation and edema) (Fig. 8)
* loss of normal architecture and height of the intervertebral disc
* T1 C+ (Gd): diffuse or rim enhancement of the intervertebral disc
- Endplate erosion and vertebral body changes (Fig. 9)
 Fig 9: MRI dorso-lumbar spine sagittal T1 (A), STIR (B), T1 FS C+ (Gd): spondylodiscitis at the level of T8-T9 with bone destruction associated with avid enhancement of the vertebral endplates and paravertebral soft tissues
Fig 9: MRI dorso-lumbar spine sagittal T1 (A), STIR (B), T1 FS C+ (Gd): spondylodiscitis at the level of T8-T9 with bone destruction associated with avid enhancement of the vertebral endplates and paravertebral soft tissues
* hypointense on T1 within the vertebral bodies correspond to bone destruction, hyperintense on T2 with loss of low signal cortex (bone marrow edema)
* T1 C+: avid enhancement of vertebral endplates
* destruction of the vertebral body with collapse
* spinal deformities (kyphosis, scoliosis)
- Paravertebral soft tissue involvement
* hyperintense on T2 paravertebral soft tissues (paraspinal muscle and surrounding soft tissues)
- Abscess formation
* fluid-filled collections (hypointense on T1, hyperintense in T2)
* localized paravertebral (commonly in the iliopsoas muscles) or epidural involvement (Fig. 10) (Fig.11)
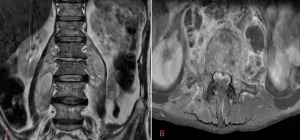
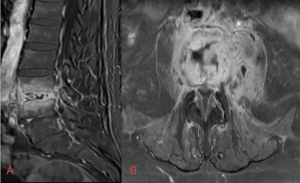
* spinal cord or nerve roots compression
* T1 C+: peripheral enhancement
Additionally, the DWI sequence can help differentiate the acute stage from the chronic stage of the disease:
* hyperintense in acute stage
* hypointense in the chronic stage
Signal and enhancement changes may persist even after clinical resolution of the infection, with these imaging findings gradually diminishing over the course of several weeks to months.
Differential diagnosis
- Modic type 1 endplate change
It can mimic spondylodiscitis due to presence of bone marrow edema, which appears hyperintense on T2 and may also show enhancement on post-contrast imaging. However, features such as endplate destruction, increased disc signal on T2 and the presence of paravertebral or epidural abscesses are specific to spondylodiscitis.
- Acute Schmorl’s node
Key distinguish features include the absence of diffuse abnormal disc signal changes, lack of peripheral nodal enhancement and preservation of the remaining vertebral endplate.
- Bone metastases
Typically appear hypointense on T1 and hyperintense on T2 with post-gadolinium enhancement. The posterior elements of the vertebrae are commonly affected and pathologic compression fractures may be present, while the disc space generally remains preserved.
- Spondyloarthropaties (reactive arthritis, psoriatic arthritis)
Absence of abscess formation and significant soft tissue involvement seen in spondylodiscitis.
- Langerhans cell histiocytosis
Imaging may reveal lytic bone lesions, often affecting the vertebral body, followed by pathological fractures. The lesions may be more focal and localized and they often do not lead to space disc narrowing. Postcontrast imaging typically shows enhancement of the lesions but lacks the peripheral enhancement or abscess formation seen in spondylodiscitis.