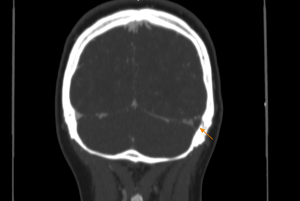
The initial radiological assessment of a lobar hemorrhage typically includes a CT scan followed by CT angiography to detect acute hemorrhages. When investigating intracranial bleeding causes after excluding intracranial aneurysms with CTA, MRI proves valuable for identifying the underlying factors both for primary and secondary ICH.
- MRI is useful in identifying primary causes (80%) of ICH, such as small-vessel disease or cerebral amyloid angiopathy. Making the distinction is essential, as it has implications on the risk of ICH recurrence, progression, and decision-making regarding the safety of antithrombotic treatments.
- MRI also plays a critical role in identifying secondary causes (20%) of ICH. These include structural vascular lesions such as arteriovenous malformations, cavernomas, or dural arteriovenous fistulae. Other readily apparent secondary causes of ICH diagnosed predominantly via MRI include hemorrhagic conversion of AIS, neoplasms, along with cerebral venous thrombosis, arterial dissection, and non-atheromatous vasculopathies.
Primary causes of intracerebral hemorrhages:
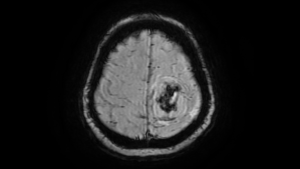
Congophilic amyloid angiopathy is progressive deposition of amyloid within small- to medium-sized blood vessels leading to fibrinoid necrosis and vascular fragility. Congophilic amyloid angiopathy is a major cause of primary lobar intracranial hemorrhage in the elderly and is a common cause of cerebral microhemorrhages. In patients older than 60 years, the diagnosis of congophilic amyloid angiopathy should be suspected if there are two or more lobar hemorrhages of any duration, areas of high signal intensity in the white matter, and multiple cerebral microhemorrhages at the corticomedullary junction. As the number of microhemorrhages increases, so does the risk for intracerebral lobar hemorrhage and associated neurologic impairment. There are no proven management options that stop or reverse Aβ deposition in CAA. Current management focuses on secondary prevention, with risk factor modification including treatment of hypertension through lifestyle modifications (smoking cessation, improved diet, and exercise) and the use of antihypertensive medication. Avoidance of anticoagulants and antiplatelet agents is generally advised as their use has been shown to increase ICH risk.
Hypertensive cerebral angiopathy is the development of intimal hyperplasia and hyalinosis in deep penetrating brain arterioles as the result of chronic systemic hypertension. These microangiopathic changes can lead to subclinical cerebral microbleeding. Unlike congophilic amyloid angiopathy, cerebral microhemorrhages associated with chronic hypertension are more commonly found in the thalamus, basal ganglia, cerebellum, and pons, sites of hypertensive intracerebral hematoma. It is postulated that hypertensive cerebral microhemorrhage is a risk factor for subsequent intracerebral hematoma.
Secondary causes of intracerebral hemorrhages:
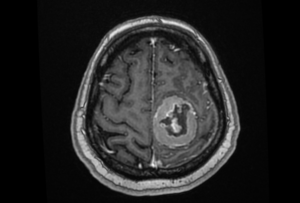
Malignant brain tumors may occasionally lead to intracranial hemorrhage. However, spontaneous hemorrhage as an initial presentation for meningioma, even though reported, is less frequent (the incidence ranges from 0.5-2.4%). The proposed mechanisms include: weakened blood vessel rupture, endothelial proliferation and resultant vascular occlusion, direct tumor cell invasion of the vasculature, bioactive substance accumulation in the tumor, concomitant vascular malformation or aneurysm. MRI usually displays dense, well-defined, contoured extra-axial masses that displace the adjacent brain along with acute or subacute hemorrhage. In addition to its diagnostic role, previous reports have provided some information on the signal intensity on MRI and have indicated hyperintensity on T2-weighted MRI as a risk factor of meningioma bleeding.
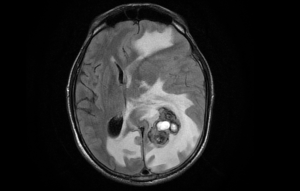
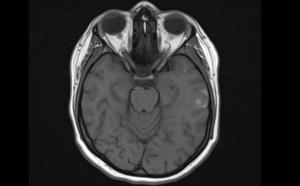
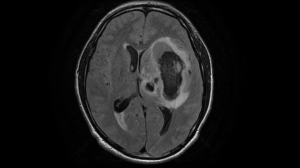
While cavernous malformations can be seen using a CT scan, they are often difficult to distinguish from other types of tumors or other vascular malformations. MRI is the most important diagnostic tool for the identification of cavernoma. The lesion characteristically displays a popcorn ball appearance involving heterogenous signal intensity core in T1 and T2 weighted and a rim of hemosiderin ring surrounding the lesion visualized as low signal intensity in T2-weighted image (T2 blooming sign). SWI is more sensitive and useful for the detection of the hemosiderin deposit and smaller lesions than conventional sequences. Cavernomas can present with atypical radiological features in cases with recent hemorrhage. These features may be characterized by vasogenic edema, mass effect on adjacent structures, loss of the hypointense peripheral hemosiderin rim, and presence of perilesional hemorrhage.

Arteriovenous malformations are a developmental anomaly of the vascular system, consisting of tangles of poorly formed blood vessels in which the feeding arteries are directly connected to a venous drainage network without any interposed capillary system. The sensitivity of computed tomography to identify brain AVMs in the acute setting of hemorrhage is reduced owing to compression of the nidus by the hematoma so more sensitive techniques such as MRI or angiography are required. MRI is very sensitive for plotting the location of the brain AVM nidus and often an associated draining vein or any distant bleeding event. Fast flow in a conglomerate of tangled blood vessels generates serpiginous and tubular flow voids seen on both T1 and T2. After radiosurgery, MRI can evaluate the regression of the nidus volume, post-therapy edema as well as radiation necrosis in the radiation field.
Dural arteriovenous fistulas are vascular abnormalities in which arteries arising from branches of the carotid or vertebral arteries drain directly into the dural leaflets of the venous sinuses. DAVFs may be benign lesions. However, due to cortical venous reflux or cortical venous obstacles, these lesions may possess aggressive manifestations (intracranial hemorrhage or a non-hemorrhagic neurological deficit). While traditional DSA is the gold standard for diagnosing and evaluating DAVFs, angiography is invasive and cannot be used to observe brain tissue or structure. Conventional magnetic resonance imaging (MRI) sequences, including MR angiography (MRA), allow the evaluation of DAVFs without ionizing radiation or invasiveness. Recently, SWI has been accepted as a new imaging modality for the detailed depiction of venous hemodynamics in vascular malformation of the brain. In patients with dAVF, dilated cerebral veins on SWI reflect venous congestion, and hyperintense signals within those veins indicate the presence of retrograde cortical venous drainage suggesting that the hemodynamic stress around the fistula is severe. Advanced MRI techniques for DAVF evaluation have demonstrated promising results not only for diagnostic purposes but also for planning therapeutic options. Dynamic contrast-enhanced MRA has become an important alternative diagnostic method and supersedes digital subtraction angiography in displaying the overall intracranial drainage pattern.
Cerebral venous infarct is an uncommon cause of all strokes (0.5–2%) that disproportionately affects young adults, most commonly caused by cerebral venous thrombosis. Approximately 50% of cerebral venous occlusions progress to CVI, which constitute rare, non-arterial distribution infarcts secondary to increases in venous pressure resulting in ischemia. If the rise in venous pressure is rapid and in the absence of adequate venous collateral recruitment, the valveless and friable cerebral veins may be unable to withstand the pressure gradient, leading to rupture of the cerebral veins and parenchymal hemorrhage. Unenhanced MR is more sensitive for the demonstration of the venous thrombus and the occluded dural sinus or vein when compared to unenhanced CT. It offers detailed cerebral vein visualization, ruling out alternate causes like bleeding or tumors.


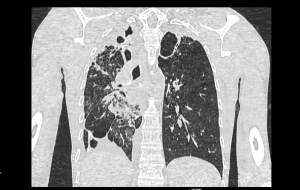
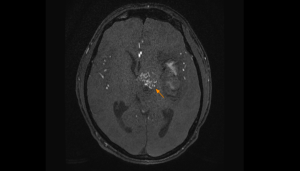
Metastases that are characterized by hemorrhage as (one) classic clinical sign include malignancies such as melanoma, choriocarcinoma, renal cell carcinoma, thyroid, lung, and breast cancer. Of all hemorrhagic metastases, however, lung and breast cancers are the most common etiologies due to their higher overall prevalence. MRI is a sensitive screening test for brain metastasis. Contrast-enhanced T1-weighted imaging is now considered to be the gold standard assessment method of brain metastases. As T2*- weighted imaging and CE-T1WI are the most commonly used MRI techniques, it is likely that only lesions with obvious haemorrhage will be identified. This can result in a relatively low detection rate for brain metastases. Susceptibility-weighted imaging is a relatively new MRI technique that allows enhancement of local contrasts, exploiting the magnetic properties of tissues that affect magnetic field inhomogeneity. The SWI technique is exquisitely sensitive to most blood products, and can detect partially deoxygenated venous blood and different blood products in haemorrhages, even in micro-haemorrhages.
The multiple hemorrhagic metastases, cavernomas, amyloid angiopathy, cerebral vasculitis, diffuse axonal injuries, and calcified neurocysticercosis all show similar SWI pictures. It is usually difficult to differentiate between these lesions based only on neuroimaging, so a tissue diagnosis is frequently needed. It is rare that hemorrhage occurs in a solitary brain metastasis. Consider hemorrhagic metastasis as a differential diagnosis in patients presenting with solitary intracerebral hemorrhage whose location is uncommon, especially when the poor general state of the patient cannot be explained by hypertensive intracerebral hemorrhage.