Results
A retrospective analysis of MRI findings from 18 patients with various lung pathologies. Among them, the following were identified:
*10 patients (55.6%) had lung formations smaller than 10 mm;
*3 patients (16.7%) had lung formations larger than 10 mm;
*1 patient (5.6%) exhibited signs of pleuropneumonia;
*1 patient (5.6%) showed paravertebral postoperative changes;
*3 patients (16.7%) had no detectable lung pathology on MRI.
Additionally, the analysis noted several cases where MRI findings were compared with CT images, highlighting the importance of understanding the differences between these two imaging modalities in lung pathology diagnosis. These four cases exemplified how MRI and CT can complement each other in differentiating certain lung conditions.
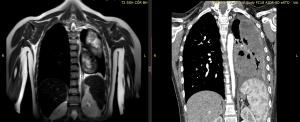
Fig 1: A 14-year-old boy with right-sided lower lobe pneumonia.
MRI scan: In the lower lobe of the right lung, an area measuring 27x12 mm is determined, with clear, uneven contours, heterogeneous structure, isointensive with hyperintensive inclusions on T2 weighted images. Locally, the pleura is moderately unevenly thickened in this area.
CT: At the S6 level of the right lung, a site of pleuropneumonic infiltration is determined, with signs of consolidation of lung tissue and traction expansion of the bronchial lumen.
Fig 2: A 16-year-old girl diagnosed with Wegener's granulomatosis.
MRI: Nodular formations with a diameter of up to 19 mm with clear, uneven contours, heterogeneous structure, hyperintensive at T2 weighted images are detected in all parts of both lungs. On the right, in the middle lobe, some of these formations (2) have decay cavities up to 8.8mm in size.
CT: In the right lung at the level S2, S3, S6, S4 and on the left in the projection S2, S4, S6, S8, S10, areas of pneumofibrosis with a density of up to 67HU, up to 1.5cm in size, and decay cavities with clear contours, sizes from 0.2 cm to 2.3 cm in diameter are revealed. In comparison with the CT from 04/13/2022, there is a decrease in the number of the above-described sites.
Fig 3: A 4-year-old boy diagnosed with acute myeloid leukemia.
MRI: In all departments, multiple nodular formations, up to 11.5 mm in diameter, with clear, even contours, hyperintensive on T2 weighted images, are noted in both pulmonary fields.
CT scan: In the parenchyma of both lungs, subpleurally and interstitially, rounded formations are determined, ranging in size from 0.4 x 0.5 cm to 0.7 x 0.8 cm, density +53HU (disseminated aspergillosis).
Fig 4: A 16-year-old girl diagnosed with Wegener's granulomatosis.
MRI: Nodular formations with a diameter of up to 19 mm with clear, uneven contours, heterogeneous structure, hyperintensive at T2 weighted images are detected in all parts of both lungs. On the right, in the middle lobe, some of these formations (2) have decay cavities up to 8.8mm in size.
CT: In the right lung at the level S2, S3, S6, S4 and on the left in the projection S2, S4, S6, S8, S10, areas of pneumofibrosis with a density of up to 67HU, up to 1.5cm in size, and decay cavities with clear contours, sizes from 0.2 cm to 2.3 cm in diameter are revealed. In comparison with the CT from 04/13/2022, there is a decrease in the number of the above-described sites.
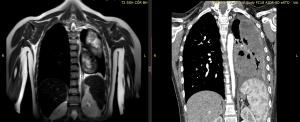
Fig 5: Girl 15 years old with osteogenic sarcoma of the left femur.
MRI: The left lung was reduced in volume due to lobectomy of the upper and resection of the lower lobe of the left lung.
In the thoracic cavity on the left, formations are determined, oval in shape, mainly of a cystic structure, with dimensions 51x57x107mm and 58x88x120mm (CT dimensions from 08/16/2022 - 126x64mm and 136x70mm), hyperintensive at T2 weighted images. The DWI and ADC maps determine the limitation of diffusion in these formations.
On the right is the pulmonary field without infiltrative and focal changes.
CT: In the left lung, oval-shaped, mainly cystic structures, multicameral formations are revealed, measuring 9.2x5.8x10.4cm (there were 10.2x7.1x13.6cm) and 6.8x5.4x10.4cm (there were 7.8x6.0x11.2cm) with clear, fairly even contours and with a uniform thick wall. The structure of the formations is heterogeneous due to air inclusions, decay cavities, hyperdense areas, and the density of the liquid component is up to +22HU. In the lower parts of the left lung, a section of the compacted pulmonary parenchyma is visualized without the presence of bronchial lumen, in all parts of the parenchyma of the left lung, reticular changes are observed. In the left pleural cavity there is liquid content, density up to +24HU, thickness up to 1.1 cm, with the presence of areas of compaction and calcification in the structure of the costal pleura in this area.
On the right is the pulmonary field without focal and infiltrative changes.
Based on the results of the analysis, it can be noted:
Advantages MRI of lungs:
- No radiation exposure: Unlike CT scans, which use ionizing radiation, MRI does not expose children to harmful radiation, making it safer, especially for repeated imaging studies.
- High soft tissue contrast: MRI provides excellent contrast between soft tissues, allowing for detailed visualization of structures within the lungs without the need for contrast agents.
- Ability to assess lung function: Functional MRI techniques can be used to assess lung function, such as ventilation and perfusion, providing valuable information about lung health.
- No sedation required in some cases: MRI scans may not always require sedation, especially in older children who can cooperate with the procedure, reducing the risks associated with anesthesia.
Disadvantages MRI of lungs :
- Lower spatial resolution: Compared to CT scans, MRI has lower spatial resolution, which may limit its ability to detect small lesions or subtle abnormalities within the lungs.
- Longer scan times: MRI scans typically take longer to acquire compared to other imaging modalities, which can be challenging for young children who may have difficulty remaining still during the procedure.
- Limited availability: MRI machines may not be as readily available as other imaging modalities, such as X-ray or CT, especially in certain regions or healthcare settings, which can lead to delays in obtaining imaging studies.
- Motion artifacts: Children, especially younger ones, may have difficulty remaining still during the MRI scan, which can result in motion artifacts and degraded image quality.