A perianal fistula is a tract that connects the lumen of anal canal or rectum with the skin of perianal region. It has a global incidence of 1-2 cases per 10,000 people per year with 2:1 male to female ratio(1) .
Most fistulas occur as a result of chronic infection or abscess in perianal region in patients with Crohn's disease(2). Fistulas can occur in patients following diverticulitis or in patients with pelvic or bowel infections. They may also be iatrogenic, post surgical, post child birth or post radiotherapy. Fistulas may occur following anal or rectal cancers or post trauma.
Pathogenesis in most cases is associated with cryptoglandular infection. In 40-60% cases who are being treated for perianal abscess the healing process leaves a perianal fistula, the disease evolving from acute to chronic phase.
MRI is the imaging investigation of choice for the evaluation of perianal fistulas due to its high soft tissue resolution, superior field of view and multiplanar capability (3). It has a sensitivity of 100% and a specificity of 86 % in perianal fistula detection(4). MRI provides detailed description of fistulous tract in relation to anal sphincters and other pelvic floor structures and tells us about any associated complications. The post surgical treatment findings can also be seen well, helping clinicians in further management. MRI T1 weighted images are good at visualizing anal sphincters, levator ani and ischiorectal fossa. On T2 weighted images, we can see the fistulous tracts with hyperintense fluid within the tracts. On contrast enhanced T1 sequence, the granulation tissue in the tract wall enhances. Any abscess in adjacent tissues shows ring enhancement and if diffusion weighted sequence is also done then abscess will show diffusion restriction. Chronic fistulae appear hypointense on T1 and T2 weighted images and show reduced or no enhancement.
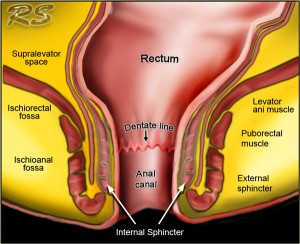
Anatomy: The anal canal extends from the perianal skin to the dentate line. Surgically the anal canal extends from the perianal skin to anorectal ring, which is formed by puborectalis muscle and lies 4-5 cm above the dentate line. The anal sphincter is comprised of 3 layers:
i. Internal sphincter: continuation of involuntary circular smooth muscle of rectum.
ii. Intersphincteric space
iii. External sphincter: Voluntary striated muscle which is continuous superiorly with puborectalis muscle and levator ani.
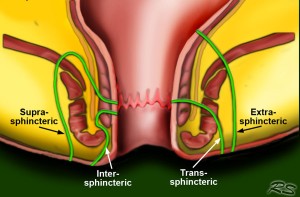
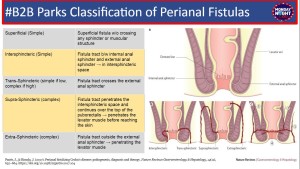
Classification of Perianal fistulas: The Surgical classification by Park's, et al (5), is based on the clinical examination by the surgeon. They have postulated 5 classes based on severity.
The radiological classification of perianal fistulas is the Saint James University Hospital Grading (6). It includes any associated complications and secondary tracts. The radiological grades are as follows:
Grade 0: Normal.
Grade 1: Simple linear Intersphincteric fistula.
Grade 2: Intersphincteric fistula with secondary fistulous tract / abscess:
Grade 3: Transsphincteric fistula.
Grade 4: Transsphincteric fistula with a secondary tract / abscess within the ischioanal or ischiorectal fossa.
Grade 5: Supralevator and translevator disease.