Diagnosis:
Ultrasonography is the modality of choice for diagnosing intussusception, featuring high sensitivity and specificity (92–100%), no radiation exposure, easy accessibility and patient comfort [2, 4]. Distinctive intussusception ultrasound sings include [3]:
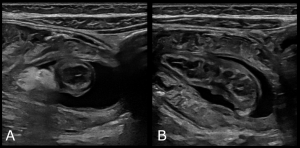
- the “target”, “doughnut” or “multiple concentric ring” sign on axial scans, formed by concentric alternating echogenic and hypoechoic bands. The echogenic bands consist of the serosa and submucosa on either side of the hypoechoic muscularis propria.
 Fig 1: Axial scans of intussusception demonstrating the characteristic “target” or “multiple concentric ring” sign. (A) Ileocolic intussusception in the left upper abdominal quadrant at the level of the left splenic flexure, containing a large hyperechoic fatty core. (B, C) Ileocolic intussusception located in the subhepatic region. (D) Small bowel intussusception in the left lateral abdomen.
Fig 1: Axial scans of intussusception demonstrating the characteristic “target” or “multiple concentric ring” sign. (A) Ileocolic intussusception in the left upper abdominal quadrant at the level of the left splenic flexure, containing a large hyperechoic fatty core. (B, C) Ileocolic intussusception located in the subhepatic region. (D) Small bowel intussusception in the left lateral abdomen. - the “pseudokidney” sign on longitudinal scans, where the mesentery, containing fat and blood vessels is pulled into the intussusception, mimicking the renal hilum, while the surrounding edematous bowel resembles renal parenchyma.
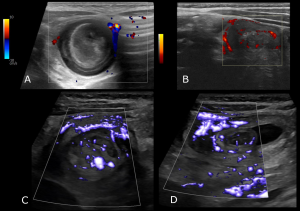
 Fig 2: Oblique scan of ileocolic intussusception forming the “pseudokidney” sign.
Fig 2: Oblique scan of ileocolic intussusception forming the “pseudokidney” sign. - the “crescent-in-doughnut" sign, the transverse equivalent of the pseudokidney sign, where the echogenic crescent is created by the mesentery.
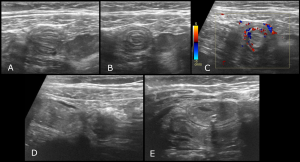
- the “sandwich” or “hayfork” sign on longitudinal scans, formed by the characteristic “bowel-within-bowel” layering.
 Fig 3: Longitudinal ultrasound images of intussusception, exhibiting the characteristic “sandwich” sign. (A) Ileoileal intussusception, (B, C) Ileocolic intussusception.
Fig 3: Longitudinal ultrasound images of intussusception, exhibiting the characteristic “sandwich” sign. (A) Ileoileal intussusception, (B, C) Ileocolic intussusception.
Additional findings may include fluid within the intussusceptum, echogenic mesenteric fat, and enlarged mesenteric lymph nodes.
Identifying the type of intussusception is essential for appropriate management. Ileocolic intussusception requires intervention and in most cases a reduction under ultrasound or fluoroscopic guidance can be performed. Key features favoring ileocolic intussusception include [1, 5]:
- a hyperechoic fatty core
 Fig 6: Ileocolic intussusception containing a prominent hyperechoic fatty core.
Fig 6: Ileocolic intussusception containing a prominent hyperechoic fatty core. - larger lesion diameter
- thicker outer hypoechoic wall
- ratio of fatty core diameter to outer wall thickness greater than 1.0
 Fig 7: Ileocolic intussusception located in the right lower quadrant, with a ratio of fatty core diameter (1.04cm) to outer wall thickness (0.41cm) greater than 1.0 (2.54).
Fig 7: Ileocolic intussusception located in the right lower quadrant, with a ratio of fatty core diameter (1.04cm) to outer wall thickness (0.41cm) greater than 1.0 (2.54). - lymph nodes within the intussusception
 Fig 8: Ileocolic intussusception containing lymph nodes within the intusscusceptum.
Fig 8: Ileocolic intussusception containing lymph nodes within the intusscusceptum. - greater lesion length
- absence of normal sonographic features of the ileocecal junction and ascending colon.
Small bowel intussusception is typically transient, but may require surgery if spontaneous reduction is unlikely, often due to the presence of pathologic lead points [1, 6].
Nonoperative enema reduction:
Nonoperative enema reduction is the treatment of choice for ileocolic intussusception in pediatric patients without signs of perforation or peritonitis, with a success rate of 82%. Its fundamental concept involves increasing intraluminal pressure in the colon using an enema, to push the invaginated small bowel back through the ileocecal valve [2]. Fluoroscopy and ultrasound are the imaging modalities employed for real-time monitoring of intussusception reduction. Fluoroscopy-guided enema typically utilizes barium, water-soluble contrast, or air, whereas the ultrasound-guided technique employs generally water or saline, and less commonly gas enemas [4].
Fluoroscopy-guided pneumatic enema achieves higher intraluminal pressure, and offers clear visualization of successful reduction, with low complication risks. However, it exposes patients to ionizing radiation, requires costly equipment, and only visualizes intraluminal content [2, 4]. Although ultrasound-guided enema achieves lower intraluminal pressure, it avoids radiation exposure, offers better recognition of pathological lead points, and detects possible differential diagnoses [2, 4, 7].
A delayed repeat enema is recommended if the initial attempt partially reduces the intussusception, provided the patient remains hemodynamically stable without signs of peritonitis. Although not clearly established, common waiting interval between attempts ranges from 15 minutes to a few hours [2].
Predisposing factors for failure of non-operative reduction include [2, 8]:
- Onset of symptoms at least 48 hours prior to diagnosis
- Younger age
- Symptoms
- Lethargy
- Bloody diarrhea
- Fever
- Septic shock – Peritonitis
- Radiologic findings
- Small bowel obstruction
- Trapped fluid within the intussusception
- Ascites
- Absence of flow in the intussusception
- Intussusception located in the left-sided colon
- Pathologic lead points