Out of 50 MRI cases analyzed, 35 were diagnosed with primary sclerosing cholangitis (PSC). Cholangitis, a condition marked by inflammation of the bile ducts, has a variety of potential etiologies, including obstructive, infectious
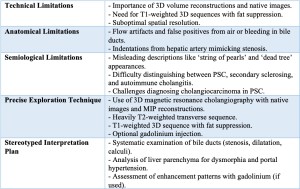
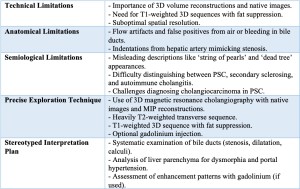
Understanding the limitations of MRI and using a structured diagnostic approach is important to avoid common traps and pitfalls in diagnosing bile duct diseases
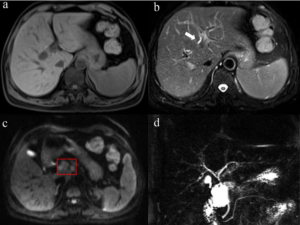
Primary Sclerosing Cholangitis (PSC)
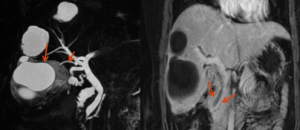
Primary sclerosing cholangitis is typically diagnosed in individuals in their 40s or 50s and is significantly associated with inflammatory bowel disease (IBD). MRCP, the gold standard imaging modality for PSC, provides detailed visualization of alternating multifocal strictures and segmental dilatations along the bile ducts, producing the characteristic beaded appearance of the disease. The involvement is typically diffuse, affecting both intrahepatic and extrahepatic bile ducts, with advanced cases showing a pruned-tree appearance due to peripheral duct atrophy. Unlike IgG4-related cholangitis, PSC is characterized by irregular strictures rather than smooth ones, and there is no periportal lymphadenopathy, which is often seen in tuberculosis cholangitis
Primary Biliary Cholangitis (PBC)
Primary biliary cholangitis (PBC) is a chronic autoimmune liver disease that primarily affects small intrahepatic bile ducts, leading to progressive cholestasis and eventual liver cirrhosis. It predominantly affects middle-aged women and is strongly associated with antimitochondrial antibodies (AMA). Unlike PSC, MRCP findings are often normal, as the disease affects microscopic bile ducts that are not well visualized on imaging. In later stages, mild bile duct pruning can be observed, along with secondary signs of cirrhosis such as a nodular liver contour and splenomegaly. The absence of large duct involvement, multifocal strictures, and the beaded appearance differentiates it from PSC and IgG4-related cholangitis
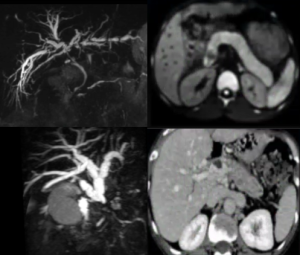
Tuberculosis Cholangitis
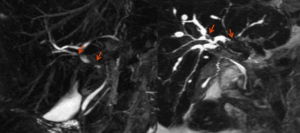
This condition often seen in patients with a history of tuberculosis or in areas where the disease is endemic. On MRCP, the disease typically presents with a beaded appearance of the bile ducts, similar to PSC, but with more irregular, abrupt strictures and shorter segments of dilatation. Additionally, confluent periductal soft tissue thickening is common, leading to external compression of the bile ducts rather than intrinsic ductal disease. Another key feature is the presence of enlarged perihilar lymph nodes, often with central necrosis, which helps differentiate it from PSC and IgG4-related cholangitis. While granulomas are not directly visible on MRCP, the imaging technique is critical for identifying bile duct abnormalities and guiding further diagnostic investigations
CT scan is beneficial in assessing the extent of biliary obstruction and can help identify complications like biliary abscesses or periductal inflammation. It also provides a broader view of surrounding structures, helping to detect lymphadenopathy and ascites, which are common in tuberculosis cholangitis. Ultrasound, on the other hand, is often the first-line imaging modality and can help detect bile duct dilatation, stricture, and obstruction. While it may not provide as detailed an image of the bile ducts as MRCP or CT, ultrasound is a non-invasive, accessible option for initial evaluation.
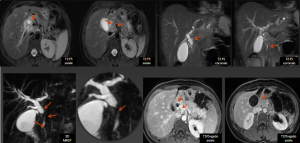
IgG4-Related Cholangitis
IgG4-related cholangitis was also diagnosed in a few cases. Imaging plays a crucial role in diagnosing and monitoring IgG4-related sclerosing cholangitis (IgG4-SC). Ultrasound (US) is often the first imaging modality used, showing circumferential bile duct wall thickening and intrahepatic duct dilatation in later stages. However, it has limited sensitivity and cannot differentiate IgG4-SC from other conditions like primary sclerosing cholangitis (PSC) or cholangiocarcinoma.
MRCP is the investigation of choice, revealing long, smooth, and concentric bile duct wall thickening that involves both intrahepatic and extrahepatic ducts. The strictures tend to be uniform and without abrupt transitions, with minimal upstream dilation, unlike the irregular strictures seen in PSC. The disease is often associated with autoimmune pancreatitis, which appears as a sausage-shaped pancreas, and can also involve the gallbladder or retroperitoneal fibrosis
The presence of these associated findings helps distinguish it from other biliary pathologies such as PSC and cholangiocarcinoma. Additionally, IgG4-SC is unique in its response to steroid therapy, often leading to significant improvement in strictures on follow-up imaging.
Other Etiologies
In addition to the more common forms of cholangitis, other etiologies should be considered in specific clinical contexts.
- Ischemic cholangitis results from impaired blood supply to the biliary tree, often due to hepatic artery thrombosis, vasculitis, or hypoperfusion. MRCP findings typically show segmental bile duct strictures, diffuse bile duct wall thickening, and peribiliary hyperintensity on T2-weighted MRI, distinguishing it from PSC, which has a more diffuse involvement.
- Drug-induced cholangitis can result from medications such as chemotherapeutic agents or antibiotics, with imaging findings that may include diffuse bile duct wall thickening, mild ductal dilatation, and periportal edema. The absence of multifocal strictures and the correlation with drug exposure aid in its differentiation from other forms of cholangitis.
- Parasitic cholangitis, caused by infections like Clonorchiasis, Echinococcus granulosus and Ascariasis, is more prevalent in endemic areas. MRCP typically reveals bile duct dilatation with intraductal filling defects representing the parasites or debris, and chronic cases may lead to periductal fibrosis and ductal strictures, mimicking other sclerosing cholangitis types.
The characteristics mentioned above are summarized in the table below