There is a wide list of primary & secondary lesions that affect the corpus callosum. Due to better soft tissue resolution, MRI is considered as a superlative diagnostic modality in evaluation of CC disorders. Callosal lesions are best seen in sagittal & coronal planes due to the anatomical shape and location.
I. Congenital lesions:
Callosal malformations:
- Include total absence (agenesis) and partial dysgenesis (only the splenium or rostrum are absent).
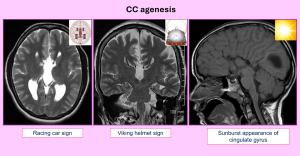
Findings of CC agenesis:
-
- Parallel, non-converging lateral ventricles giving a racing car appearance on axial images.
- Colpocephaly (dilated occipital horns).
- Dilated high-riding 3rd ventricle.
- Probst bundles indenting the lateral ventricles resembling a viking helmet on coronal images.
- Absent or everted cingulate gyrus giving "sunray appearance" in sagittal plane.
- Callosal dysgenesis is associated with other anomalies (Chiari II, migration disorders, Dandy Walker malformation, holoprosencephaly)(3).
Pericallosal lipoma:
- Tubulonodular type:located anteriorly, > 2 cm, associated with encephaloceles & frontal lobe anomalies.
- Curvilinear type:posterior, thinner, ribbon-like, < 1 cm, usually arch around the splenium(4).
 Fig 3: Sagittal T1W images demonstrate the types of pericallosal lipoma associated with variable degrees of CC dysgenesis.(@Radiopaedia cases).
Fig 3: Sagittal T1W images demonstrate the types of pericallosal lipoma associated with variable degrees of CC dysgenesis.(@Radiopaedia cases).
II. Hereditary disorders:
1. X-Linked adrenoleukodystrophy
- Presentaion:seizures, visual–behavioral disturbances, mental retardation.
- Adrenal insufficiency & undescended testis may coexist.
- Periventricular WM with posterior-predominant pattern and early involvement of splenium(5).
- Lesions appear hyperintense on FLAIR &T2WI, hypointense on T1WI.
- The peripheral zone of demyelination shows restricted diffusion on DWI and serpiginous enhancement (may indicate disease progression).
 Fig 4: A case of X-linked adrenoleukodystrophy with bilateral nearly symmetrical parieto-occipital WM hyperintensity at T2WI (A) and FLAIR (B). Enhancement of the leading edge of active demyelination is noted in T1WI+C (yellow arrows in C). Involvement of the splenium is noted (blue arrows in B & C).© '' Radiology Department, Mansoura University Hospitals''.
Fig 4: A case of X-linked adrenoleukodystrophy with bilateral nearly symmetrical parieto-occipital WM hyperintensity at T2WI (A) and FLAIR (B). Enhancement of the leading edge of active demyelination is noted in T1WI+C (yellow arrows in C). Involvement of the splenium is noted (blue arrows in B & C).© '' Radiology Department, Mansoura University Hospitals''.
2. Krabbe disease
- Presentaion of early-onset type:spasticity, irritability, fever, and developmental delay.
- Location:cerebellar WM, thalami, dentate nuclei, lentiform, and corticospinal tracts(1).
 Fig 5: Krabbe's disease. MRI shows high signal intensity along the pyramidal tract in the posterior limb of internal capsule (arrows in A), crus cerebri (double arrows in B), demonstrated on FLAIR (A) and T2WI (B). Similar signals are seen in the peritrigonal white matter (arrowheads in A) and splenium of corpus callosum (double arrows in A).(@Kazi AZ, et al. (2013) MRI evaluation of pathologies affecting the corpus callosum: A pictorial essay. Indian J Radiol Imaging;23(4):321-32).
Fig 5: Krabbe's disease. MRI shows high signal intensity along the pyramidal tract in the posterior limb of internal capsule (arrows in A), crus cerebri (double arrows in B), demonstrated on FLAIR (A) and T2WI (B). Similar signals are seen in the peritrigonal white matter (arrowheads in A) and splenium of corpus callosum (double arrows in A).(@Kazi AZ, et al. (2013) MRI evaluation of pathologies affecting the corpus callosum: A pictorial essay. Indian J Radiol Imaging;23(4):321-32). - High T2 /FLAIR signal involving parieto-occipital predominant or diffuse periventricular WM involvement (tigroid pattern).
- Subcortical U-fiber are spared until late.
3. Metachromatic leukodystrophy
- Bilateral symmetrical confluent areas of periventricular deep WM high T2 & FLAIR signal, particularly around the atria & frontal horns (butterfly pattern).
- Tigroid pattern on axial or leopard pattern on sagittal plane representing sparing the venules.
- Subcortical-U fibers are spared(6).
 Fig 6: MRI features of metachromatic leukodystrophy.(@Radiopaedia cases).
Fig 6: MRI features of metachromatic leukodystrophy.(@Radiopaedia cases).
III. Acquired lesions:
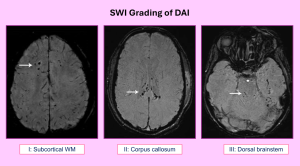
A) Traumatic (diffuse axonal injury)
- Sudden acceleration-deceleration or rotational forces, which cause axonal shear-strain deformations.
- Hemorrhagic foci are best depicted on T2*(GRE) or SWI.
- DWI:can be either vasogenic / cytotoxic edema or hemorrhagic lesion.
 Fig 7: A healthy 22-year-old individual with history of a road traffic accident. Axial FLAIR (A) shows multiple subcortical white matter and corona radiata hyperinstense lesions, with diffuse hyperintensity and mild swelling of the splenium. Axial DWI (B) shows diffuse periventricular white matter and CC diffusion restriction. Sagittal T2WI (C) shows the splenial signal abnormality. (@Machnowska M , et al(2015). AJNR cases).
Fig 7: A healthy 22-year-old individual with history of a road traffic accident. Axial FLAIR (A) shows multiple subcortical white matter and corona radiata hyperinstense lesions, with diffuse hyperintensity and mild swelling of the splenium. Axial DWI (B) shows diffuse periventricular white matter and CC diffusion restriction. Sagittal T2WI (C) shows the splenial signal abnormality. (@Machnowska M , et al(2015). AJNR cases).
DAI Grading system(7): is summarized in figure (8).
B) Ischemic
- Exclusive CC infarcts are rare due to rich blood supply.
- Associations:systemic vasculitides, shower emboli, large vessel occlusion or subfalcine herniation(8).
- Location:splenium (most common), followed by body & genu.
- N.B:hypoxic-ischemic encephalopathy: CC is involved in severe cases.
 Fig 9: A case of hypoxic ischemic encephalopathy (HIE) in a 13-day-old baby with asphyxia and respiratory distress. MRI shows restricted diffusion in the entire corpus callosum (arrows in A-D) on DWI (A, C) and ADC images (B, D).(@Kazi AZ, et al. (2013) MRI evaluation of pathologies affecting the corpus callosum: A pictorial essay. Indian J Radiol Imaging;23(4):321-32).
Fig 9: A case of hypoxic ischemic encephalopathy (HIE) in a 13-day-old baby with asphyxia and respiratory distress. MRI shows restricted diffusion in the entire corpus callosum (arrows in A-D) on DWI (A, C) and ADC images (B, D).(@Kazi AZ, et al. (2013) MRI evaluation of pathologies affecting the corpus callosum: A pictorial essay. Indian J Radiol Imaging;23(4):321-32).
C) Retinocochleocerebral Vasculopathy (Susac syndrome):
- Small infarctions of cochlear, retinal, encephalic tissue (SICRET).
- Female patients (20-40 years) with CC lesions and clinical triad (encephalopathy, bilateral SNHL, branch retinal artery occlusions).
- T2/ FLAIR hyperintense lesions at CC body & splenium. May involve brainstem, BG, thalamus, subcortical WM, centrum semiovale(9).
 Fig 10: Susac syndrome: clinical triad and characteristic snowball sign of CC involvement.(@Rennebohm R, et al.(2010) Susac's Syndrome--update. J Neurol Sci;299(1-2):86-91).
Fig 10: Susac syndrome: clinical triad and characteristic snowball sign of CC involvement.(@Rennebohm R, et al.(2010) Susac's Syndrome--update. J Neurol Sci;299(1-2):86-91).
D)Vascular
1.Arteriovenous Malformations
- AVM of the corpus callosum represents 9-11% of all cerebral AVM.
- May cause hematoma in CC itself, often with intraventricular hemorrhage.
- MRI:serpentine flow voids at the corpus callosum & ventricles +/- I.V.H(10).
2.Aneurysm
- Midline & parasagittal aneurysms can occasionally rupture into CC. These usually arise from distal ACA or ACOM(8).
 Fig 11: (A): T2* GRE image verifies blooming in a lobulated collection suggestive of acute hematoma in midfrontal region, involving genu of corpus callosum. (B): TOF-MRA image depicts T1-hyperintense hematoma (asterisk) surrounding ruptured anterior communicating artery aneurysm.(@Ho ML, et al. (2013) Lesions of the corpus callosum. AJR)
Fig 11: (A): T2* GRE image verifies blooming in a lobulated collection suggestive of acute hematoma in midfrontal region, involving genu of corpus callosum. (B): TOF-MRA image depicts T1-hyperintense hematoma (asterisk) surrounding ruptured anterior communicating artery aneurysm.(@Ho ML, et al. (2013) Lesions of the corpus callosum. AJR) - Callosal hematoma is associated with SAH mainly in interhemispheric cistern.
3.Virchow-Robin spaces
- Dilated perivascular spaces that can occur in cerebral WM, including CC.
- Ovoid lesions isointense to CSF.
- Association:mucopolysaccharidosis(8).
 Fig 12: Dilated Virchow-Robin spaces in Hunter syndrome (mucopolysaccharidosis type 2). (A): Axial FLAIR image shows diffusely enlarged perivascular spaces, which are isointense to CSF and involve body of corpus callosum (arrows). (B): Sagittal T1 FLAIR contrast-enhanced image shows large VRS within corpus callosum (arrow) and brain parenchyma.(@Ho ML, et al. (2013) Lesions of the corpus callosum. AJR)
Fig 12: Dilated Virchow-Robin spaces in Hunter syndrome (mucopolysaccharidosis type 2). (A): Axial FLAIR image shows diffusely enlarged perivascular spaces, which are isointense to CSF and involve body of corpus callosum (arrows). (B): Sagittal T1 FLAIR contrast-enhanced image shows large VRS within corpus callosum (arrow) and brain parenchyma.(@Ho ML, et al. (2013) Lesions of the corpus callosum. AJR)
E)Demyelinating Diseases
1. MS
- Lesions involve periventricular WM, internal capsule, CC, and pons.
- MRI:thin, ovoid, flame-shaped lesions (Dawson's fingers), oriented perpendicular to lateral ventricles.
- Calloso-septal interface is highly specific for MS(3).
- Sagittal, thin-section, FLAIR images are useful for lesion detection.
 Fig 13: (A) Sagittal FLAIR shows multiple high signal plaques at the callososeptal interface (considered specific for MS). (B): Axial FLAIR demonstrates multiple typical extra-callosal lesions (periventricular and juxta-cortical).(@ECR 2019 / C-3222).
Fig 13: (A) Sagittal FLAIR shows multiple high signal plaques at the callososeptal interface (considered specific for MS). (B): Axial FLAIR demonstrates multiple typical extra-callosal lesions (periventricular and juxta-cortical).(@ECR 2019 / C-3222). - DD:from ischemia, trauma, other demyelinating diseases via morphology, location, concurrent MS plaques in periventricular WM.
2. Neuromyelitis Optica (NMO)
- Usually presents as optic neuritis or longitudinally extensive spinal cord lesion.
- Location of brain lesions:periependymal regions, periaqueductal GM,medial thalamus, dorsal pons/medulla and CC.
- Marbled pattern of CC (multiple overlapping lesions with heterogeneous signal)(11)has been described in the acute phase.This is distinct from MS (smaller separate lesions seen at calloso-septal interface).
3. Progressive multifocal leukoencephalopathy (PML)
- Reactivation of (JC virus) in immunocompromised patients.
- MRI:multifocal lesions of low T1, high T2 & FLAIR signal, asymmetric periventricular & subcortical involvement. Peripheral patchy diffusion restriction at the leading edge.
- Predilection for parieto-occipital regions.
- CC lesions can enlarge & become confluent with disease progression(10).
- Barbell sign:parieto-occipital signal crossing the splenium.
- Shrimp sign:cerebellar WM involvement sparing the dentate nucleus.
 Fig 14: MRI features of PML in HIV positive patients. (A): Axial FLAIR shows scalloped high signal intensity lesions in the right occipital lobe with contralateral extension across the corpus callosum. (B): Axial T2WI shows high signal intensity of the cerebellar WM sparing the dentate nucleus. (C): Axial ADC map of another patient showing peripheral restricted diffusion (white arrow) of the left parieto-occipital lesion.(@Radiopaedia cases).
Fig 14: MRI features of PML in HIV positive patients. (A): Axial FLAIR shows scalloped high signal intensity lesions in the right occipital lobe with contralateral extension across the corpus callosum. (B): Axial T2WI shows high signal intensity of the cerebellar WM sparing the dentate nucleus. (C): Axial ADC map of another patient showing peripheral restricted diffusion (white arrow) of the left parieto-occipital lesion.(@Radiopaedia cases). - Lack of mass effect or enhancement differentiates it from SOL in HIV patients.
- Symmetrical involvement, sparing subcortical U-fibers and brain atrophy are distinctive of HIV encephalopathy.
F) Metabolic
Marchiafava-Bignami Disease (MBD)
- Most often seen with chronic alcoholism.
- 3 forms: a fulminate acute form or subacute and chronic forms.
- Location:the acute form affects the genu & splenium, whereas the chronic affects the body partcularly the central layer, sparing the upper & lower edges giving a (sandwich sign).
 Fig 15: Sandwich sign of Marchiafava-Bignami disease due to involvement of the central layer with relative sparing of the dorsal and ventral layers of the corpus callosum as shown in sagittal T1WI (A) and T2WI (B).(@Mogal V, et al. (2015). Marchiafava-Bignami Disease – A Case Report and a Brief Review of Literature.IJSR)
Fig 15: Sandwich sign of Marchiafava-Bignami disease due to involvement of the central layer with relative sparing of the dorsal and ventral layers of the corpus callosum as shown in sagittal T1WI (A) and T2WI (B).(@Mogal V, et al. (2015). Marchiafava-Bignami Disease – A Case Report and a Brief Review of Literature.IJSR) - Acute phase: patients present with sudden onset of altered consciousness, seizures, ataxia, pyramidal signs. On MRI:CC shows diffuse swelling with high T2 signal & restricted diffusion.
- Chronic phase:patients present with progressive dementia & interhemispheric disconnection. On MRI:diffuse callosal atrophy with multiple areas of focal necrosis (cavitary lesions) with high or low T2 signal (hemosiderin deposits)(3).
G) Neoplastic
1. GBM
- Location:supratentorial WM and spreads along the corpus callosum with bihemispheric involvement “butterfly” pattern.
- MRI:tumor is heterogeneously T1 hypointense & T2 hyperintense due to necrosis, hemorrhage with inhomogeneous enhancement of the solid portion(8).
 Fig 16: A case of GBM. Axial T2WI shows necrotic infiltrating mass with extension across the corpus callosum and with surrounding vasogenic edema. Axial T1WI precontrast (B) and axial T1WI postcontrast (C) demonstrate heterogeneous enhancement of this lesion. (@ Yang Y, et al. (2021) Differential Diagnosis of Corpus Callosum Lesions: Beyond the Typical Butterfly Pattern @RadioGraphics).
Fig 16: A case of GBM. Axial T2WI shows necrotic infiltrating mass with extension across the corpus callosum and with surrounding vasogenic edema. Axial T1WI precontrast (B) and axial T1WI postcontrast (C) demonstrate heterogeneous enhancement of this lesion. (@ Yang Y, et al. (2021) Differential Diagnosis of Corpus Callosum Lesions: Beyond the Typical Butterfly Pattern @RadioGraphics).
2. Gliomatosis cerebri
- A slowly growing diffuse form of glioma that infiltrates two or more lobes with no or minimal enhancement.
3. Lymphoma
- MRI:relatively low T2 signal, restricted diffusion & homogeneous enhancement.
- Locations:CC, deep GM structures, periventricular region.
- DD from GBM: less peritumoral edema, more commonly multiple, less commonly necrotic, highly radiosensitive, temporarily respond dramatically to steroid “vanishing lesions(10).
 Fig 17: A case of primary CNS lymphoma. (A): Axial T2WI shows low T2 signal mass crossing the corpus callosum. (B): Axial DWI shows restricted diffusion pattern of the mass. (C): Axial precontrast T1WI and postcontrast T1WI(D) show avid homogenous enhancement of the mass.(@Radiopaedia cases).
Fig 17: A case of primary CNS lymphoma. (A): Axial T2WI shows low T2 signal mass crossing the corpus callosum. (B): Axial DWI shows restricted diffusion pattern of the mass. (C): Axial precontrast T1WI and postcontrast T1WI(D) show avid homogenous enhancement of the mass.(@Radiopaedia cases).
4. Metastasis
- Metastasis to CC is rare. More frequently, there is contiguous extension of tumor from adjacent structures as the cingulate gyrus(12). Imaging features depend on the primary tumor.
 Fig 18: Intracranial metastases from primary lung cancer. Contrast-enhanced T1-WI shows heterogeneously enhancing dominant metastasis in left frontal lobe (asterisk). Additional enhancing foci are noted in splenium (S), genu (G), and periventricular regions (arrows).(@Ho ML, et al. (2013) Lesions of the corpus callosum. AJR).
Fig 18: Intracranial metastases from primary lung cancer. Contrast-enhanced T1-WI shows heterogeneously enhancing dominant metastasis in left frontal lobe (asterisk). Additional enhancing foci are noted in splenium (S), genu (G), and periventricular regions (arrows).(@Ho ML, et al. (2013) Lesions of the corpus callosum. AJR).
5. Germinoma
- Usually arise from the pineal or suprasellar region.
- The inferior surface of CC may be involved when ependymal/subependymal dissemination occurs(12).
 Fig 19: A case of pineal germinoma. Sagittal contrast- enhanced T1-WI shows avidly enhancing mass in pineal gland region which extends into 3rd ventricle anteriorly and invades splenium of corpus callosum (arrow) and tectum inferiorly.(@Park SE, et al. (2017) Splenial Lesions of the Corpus Callosum: Disease Spectrum and MRI Findings. Korean J Radiol.;18(4):710-721).
Fig 19: A case of pineal germinoma. Sagittal contrast- enhanced T1-WI shows avidly enhancing mass in pineal gland region which extends into 3rd ventricle anteriorly and invades splenium of corpus callosum (arrow) and tectum inferiorly.(@Park SE, et al. (2017) Splenial Lesions of the Corpus Callosum: Disease Spectrum and MRI Findings. Korean J Radiol.;18(4):710-721).
6. Meningioma
- When arising from midline & parasagittal dural surfaces, meningioma can secondarily involve the CC(8).
 Fig 20: A case of meningioma. Well-circumscribed mass centered in the falx cerebri and extending across midline and crossing the corpus callosum splenium. There is subtle surrounding edema that involves bilateral occipital regions.T1W contrast-enhanced MR image shows relatively homogeneous contrast enhancement within mass, which deviates surrounding pial vessels (arrows).(@Ho ML, et al. (2013) Lesions of the corpus callosum. AJR).
Fig 20: A case of meningioma. Well-circumscribed mass centered in the falx cerebri and extending across midline and crossing the corpus callosum splenium. There is subtle surrounding edema that involves bilateral occipital regions.T1W contrast-enhanced MR image shows relatively homogeneous contrast enhancement within mass, which deviates surrounding pial vessels (arrows).(@Ho ML, et al. (2013) Lesions of the corpus callosum. AJR).
H) Infections
- Callosal TB and aspergillosis have been reported.
- Various agents such as influenza, rotavirus, mumps, E.coli, adenovirus can cause transient splenial lesion(13).
I) Miscellaneous Lesions
1. Transient splenial lesion
- Cytotoxic lesions of corpus callosum (CLOCCs).
- Seen in patients with seizures, on antiepileptic drugs or metabolic disturbances, although many other etiologies are recognized.
- MRI:well-circumscribed, small, oval lesions within the splenium with restricted diffusion(14).
- Boomerang sign:extensive irregular lesions extending throughout the splenium into the adjacent hemispheres.
- Signal changes are usually reversible (recover completely within 1 month).
 Fig 21: MRI findings in cytotoxic lesions of the corpus callosum. A case of a 38-year-old patient who presents with a typical (CLOCC) after head trauma. (A): DWI: oval hyperintensity throughout the splenium and into the adjacent hemispheres (“boomerang sign”). (B): ADC hypointensity due to restricted diffusion. Lesion shows high signal in FLAIR (C) and T2WI (D). (E) precontarst T1WI shows a slight hypointensity. (F) post contrast T1WI shows no enhancement.(@Moors S, et al.(2024) Cytotoxic lesions of the corpus callosum: a systematic review. Eur Radiol 34, 4628–4637).
Fig 21: MRI findings in cytotoxic lesions of the corpus callosum. A case of a 38-year-old patient who presents with a typical (CLOCC) after head trauma. (A): DWI: oval hyperintensity throughout the splenium and into the adjacent hemispheres (“boomerang sign”). (B): ADC hypointensity due to restricted diffusion. Lesion shows high signal in FLAIR (C) and T2WI (D). (E) precontarst T1WI shows a slight hypointensity. (F) post contrast T1WI shows no enhancement.(@Moors S, et al.(2024) Cytotoxic lesions of the corpus callosum: a systematic review. Eur Radiol 34, 4628–4637).
2. Focal splenial gliosis
- Linear high T2/ FLAIR signal in the anteroinferior portion of the splenium.
- Occurs in patients with small-vessel ischemic disease secondary to aging, subcortical arteriosclerotic encephalopathy, or radiation therapy(12).
- Associated with periventricular & deep WM hyperintensities.
3. Wallerian degeneration
- Cerebral infarction or mass can produce atrophy of the intervening CC due to degeneration of its fibers(12).
- DWI is sensitive for early detection. Callosal atrophy occurs in chronic stage.
 Fig 22: Wallerian degeneration of the corpus callosum in a 17-year-old girl with an anaplastic astrocytoma. (A) axial post contarst T1WI shows a large right occipital heterogeneously enhancing mass. (B):sagittal T1WI obtained 6 days after surgery shows a normal corpus callosum. (C): sagittal T1WI obtained 6 years after surgery with the posterior half of the corpus callosum is markedly atrophic (yellow arrows). (@Uchino A, et al. (2006)Acquired lesions of the corpus callosum: MR imaging. Eur Radiol 16, 905–914).
Fig 22: Wallerian degeneration of the corpus callosum in a 17-year-old girl with an anaplastic astrocytoma. (A) axial post contarst T1WI shows a large right occipital heterogeneously enhancing mass. (B):sagittal T1WI obtained 6 days after surgery shows a normal corpus callosum. (C): sagittal T1WI obtained 6 years after surgery with the posterior half of the corpus callosum is markedly atrophic (yellow arrows). (@Uchino A, et al. (2006)Acquired lesions of the corpus callosum: MR imaging. Eur Radiol 16, 905–914).
4. Post shunt decompression in chronic hydrocephalus
- Prolonged lateral ventriculomegaly leads to CC stretching & impingement against rigid falx cerebri, resulting in chronic ischemia. Rapid decompression of long-standing hydrocephalus results in transcallosal demyelination.
- MRI:new enlargement with low T1 & high T2 signal in the body of CC without associated symptoms.
- Scalloped appearance of the rostral surface due to segmental tethering by pericallosal artery branches (3).
- Relative sparing of splenium.
 Fig 23: Post shunt decompression of chronic hydrocephalus. An 8-year-old female with tectal glioma (arrow in A, axial FLAIR) causing obstructive hydrocephalus, underwent an MRI for follow-up 7 days after palliative shunt decompression. The corpus callosum appears redundant with irregular rostral margins and focal signal abnormalities, which appear hypointense on T1WI (B) and hyperintense on FLAIR image (C).(@Kazi AZ, et al. (2013) MRI evaluation of pathologies affecting the corpus callosum: A pictorial essay. Indian J Radiol Imaging;23(4):321-32).
Fig 23: Post shunt decompression of chronic hydrocephalus. An 8-year-old female with tectal glioma (arrow in A, axial FLAIR) causing obstructive hydrocephalus, underwent an MRI for follow-up 7 days after palliative shunt decompression. The corpus callosum appears redundant with irregular rostral margins and focal signal abnormalities, which appear hypointense on T1WI (B) and hyperintense on FLAIR image (C).(@Kazi AZ, et al. (2013) MRI evaluation of pathologies affecting the corpus callosum: A pictorial essay. Indian J Radiol Imaging;23(4):321-32).