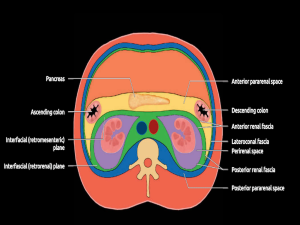
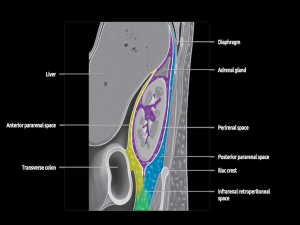
The perirenal space, or perinephric space, is the largest of the three divisions of the retroperitoneum, bounded by the anterior and posterior renal fascia, which separate it from the anterior and posterior pararenal spaces. It encompasses the kidneys, adrenal glands, perinephric fat, proximal ureters, renal vessels, and lymphatics. [1]
The first step in evaluating perinephric masses is determining the anatomical origin of the lesion, which can sometimes be obscured in cases of large, invasive lesions.
Diseases of the perirenal space often originate from renal pathology, including neoplasia, inflammation, infection, or hemorrhage. Less commonly, conditions like retroperitoneal sarcomas or inflammatory processes such as retroperitoneal fibrosis may extend into this space.
Tumors:
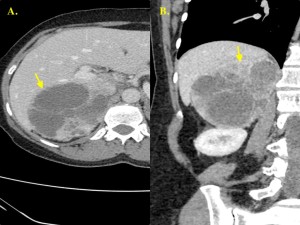
I. Renal Cell Carcinoma (RCC) [2, 3, 16, 17]
Renal cell carcinoma is the most common primary malignancy of the kidney in adults. It has three main histological subtypes: clear-cell RCC (ccRCC), papillary RCC (pRCC) and chromophobe RCC.
- NECT findings:
- Solid lesions with attenuation values of 20-70 Hounsfield Units (HU).
- Frequently heterogeneous due to necrosis, cystic degeneration or hemorrhage.
- Calcifications may be present, appearing as amorphous or curvilinear deposits.
- CECT findings:
- Variable enhancement, generally less than renal cortex.
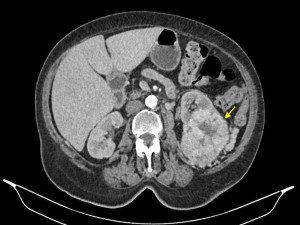
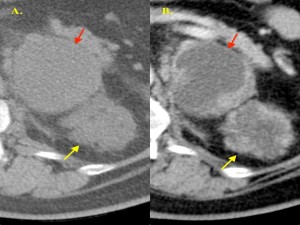
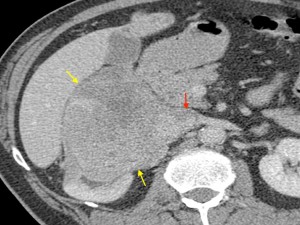
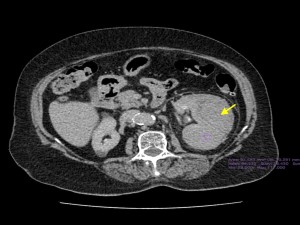
- ccRCC: usually hypervascular with marked enhancement in the corticomedullary phase. (Figure 3)
Although perinephric involvement is less commonly observed, it may be associated with advanced or bulky RCCs. Imaging findings suggestive of perirenal fat invasion include:
- Ill-defined margins between tumor and adjacent perinephric fat.
- Perinephric fat stranding.
- Thickened perirenal fascia.
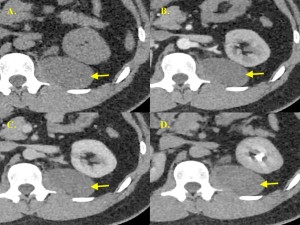
II. Lymphoma [3-6, 17]
Renal involvement by lymphoma is usually secondary to systemic disease, most often non-Hodgkin’s lymphoma.
It can present in various patterns on CT, including:
- Multiple renal masses.
- Solitary renal mass.
- Renal invasion from retroperitoneal disease.
- Perinephric disease.
- Diffuse renal infiltration.
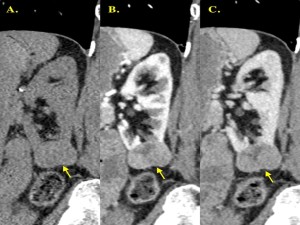
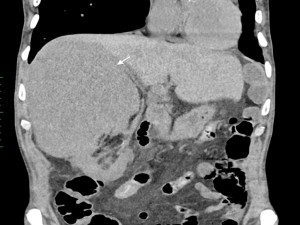
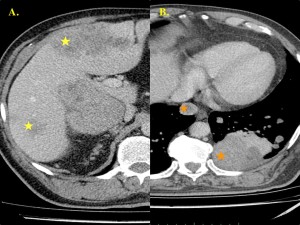
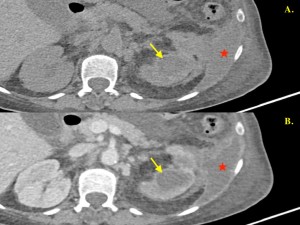
Perinephric lymphoma is a distinct pattern of renal involvement, characterized by homogeneously hypovascular and mildly enhancing soft tissue masses. It often encases retroperitoneal vessels without causing obstruction or significant stenosis, even in the presence of bulky disease.
Evidence of systemic involvement, such as splenic lesions or distant lymphadenopathy, can further support the diagnosis. However, when imaging is inconclusive, histopathological confirmation is often required.

III. Retroperitoneal Sarcoma [3, 6, 7, 16]
Retroperitoneal tumors may involve the perinephric space through direct contiguous extension.
The majority of primary retroperitoneal sarcomas fall into three main histological categories:
- Liposarcoma.
- Leiomyosarcoma.
- Undifferentiated Pleomorphic Sarcoma.
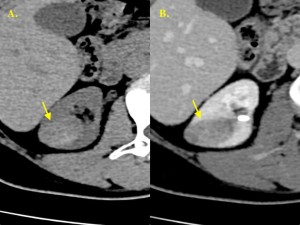
- Liposarcoma
Liposarcoma is the most common primary retroperitoneal sarcoma in adults, originating from retroperitoneal fat.
- Imaging findings:
- Fat-containing tumors with varying degrees of soft tissue components, depending on cellular atypia:
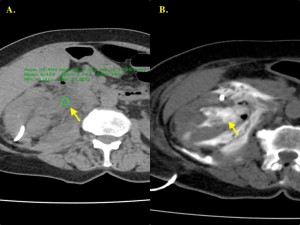
- Low-grade: Predominantly fatty lesions with minimal soft tissue. (Figure 8)
- High-grade: Dense, heterogeneous masses with significant enhancing soft tissue components. (Figure 7)
- Calcification or ossification indicate a poor prognosis.
- Fat-containing tumors with varying degrees of soft tissue components, depending on cellular atypia:
In well-differentiated fatty masses, careful evaluation is essential to identify defects in the renal capsule, which are more indicative of angiomyolipoma than liposarcoma.
- Leiomyosarcoma
Leiomyosarcoma is the second most common primary retroperitoneal sarcoma in adults, originating from the smooth muscle of vessels, renal capsule, renal pelvis, calyces, or embryological remnants in the retroperitoneum.
- Imaging findings:
- Large, heterogeneous masses with extensive necrotic and cystic changes.
- Typically located near the IVC.
IV. Metastases [1, 3, 18, 19]
Metastatic disease rarely involves the perinephric space but it can be associated with malignancies such as melanoma, prostate cancer, breast cancer, and gastrointestinal tumors. Perinephric metastases typically present as multiple discrete soft tissue masses. A history of a known primary malignancy and evidence of metastases in other locations can aid in establishing the diagnosis.
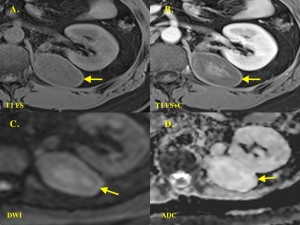
V. Angiomyolipoma (AML) [1, 3]
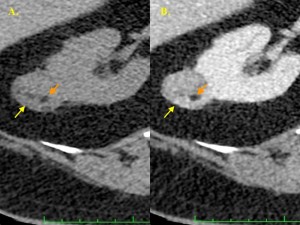
Angiomyolipoma is a benign renal tumor composed of abnormal blood vessels, smooth muscle, and adipose tissue. These tumors are often incidental findings but are associated with a risk of hemorrhage, particularly when larger than 4 cm.
- Imaging findings:
- Presence of intratumoral macroscopic fat is nearly pathognomonic.
- Lipid-poor AMLs (up to 5% of all AMLs) may complicate diagnosis. (Figure 13)
- As AMLs primarily arise from the renal parenchyma, they can often be distinguished from liposarcomas by specific imaging signs, such as the “beak sign” (divot at the kidney-mass interface) and the presence of a perforating feeding vessel.

VI. Pheochromocytoma [1, 3, 8, 16]
Pheochromocytoma is a catecholamine-producing tumor originating from the adrenal medulla.
- NECT findings:
- Appears as soft tissue density masses (>10 HU).
- Can be homogeneous or heterogeneous, with cystic or necrotic areas and occasional calcifications.
- CECT findings:
- Marked enhancement due to abundant vascularity.
- Enhancement >130 HU strongly suggests pheochromocytoma.
Imaging aids in detection, but definitive diagnosis relies on clinical history and biochemical evidence (elevated catecholamine levels)
VII. Retroperitoneal Neurogenic Tumor [1, 9, 16, 19]
Retroperitoneal neurogenic tumors, such as schwannomas, are rare neoplasms originating from Schwann cells. They are typically found in paravertebral regions near the kidneys, or in the presacral space.
- Clinical presentation:
- Often asymptomatic but may cause symptoms from compression of adjacent structures, depending on size and location.
- Imaging findings:
- Sharply circumscribed, fusiform, or oval enhancing masses.
- Usually homogeneous but can display variability due to cystic degeneration, hemorrhage or calcifications.
Other masses:
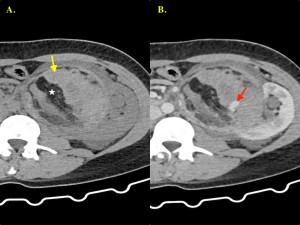
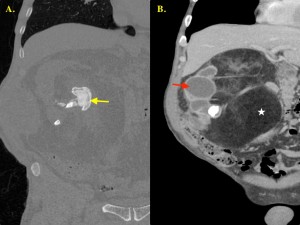
VIII. Hematomas [10, 19]
Renal hemorrhage can occur in various locations, including intraparenchymal, subcapsular, perinephric or pararenal spaces. Retroperitoneal bleeding is classified as either traumatic or nontraumatic, with nontraumatic causes subdivided into spontaneous or iatrogenic.
Spontaneous perinephric hematomas have been associated with conditions such as angiomyolipoma, renal cell carcinoma and polycystic kidney disease.
- NECT findings:
- Recent perirenal hemorrhage: high-attenuation (50-90 HU).
- Subcapsular hematomas: crescentic masses with higher attenuation than adjacent renal parenchyma; kidney flattening and elevation of the renal capsule due to pressure from the hematoma
IX. Abscesses [1, 19]
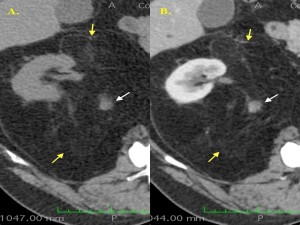
Renal abscesses are well-defined lesions on CT, typically showing attenuation values of around 30 HU.
- Imaging findings:
- Thick, enhancing walls with non-enhancing contents (pus).
- Occasionally, gas may be present within the abscess.
- Focal thickening of adjacent renal fascia and perinephric fat stranding.
- If the infection extends beyond the renal capsule, it may result in a perinephric abscess.
X. Urinomas [1, 16]
Urinomas are collections of urine within the perinephric space, commonly caused by trauma, urinary obstruction, or post-instrumentation.
- NECT findings:
- Attenuation values similar to water (0 to +10 HU).
- Delayed-phase CECT:
- Highlights extravasation of excreted contrast material, distinguishing urinomas from other fluid collections.
Inflammation:
XI. Xanthogranulomatous Pyelonephritis (XGP) [11, 19]
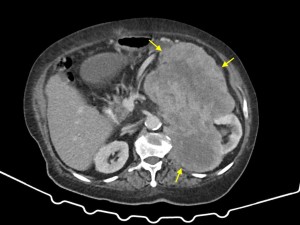
Xanthogranulomatous pyelonephritis is a rare, chronic granulomatous inflammatory condition characterized by extensive renal parenchymal destruction. It typically presents as a unilateral diffuse process.
- CT findings:
- Staghorn calculus.
- Dilated calyces (creating a multiloculated appearance referred to as the "bear's paw sign").
- Diffuse reniform enlargement with cortical thinning.
- Absence or significant reduction of renal excretion of contrast material.
- Less common manifestation: small, contracted kidney with replacement lipomatosis.
The inflammatory process may extend beyond the kidney, affecting the perinephric and pararenal spaces and occasionally involving the ipsilateral psoas muscle, diaphragm, or skin.
Proliferative Diseases
XII. Retroperitoneal Fibrosis (RPF) [12, 13, 17, 19]
Retroperitoneal fibrosis is a rare condition characterized by proliferation of fibro-inflammatory tissue, typically encasing the infrarenal portion of the great vessels (aorta, inferior vena cava and iliac vessels).
- CT findings:
- Appears as a soft tissue density mass surrounding the infrarenal aorta anterolaterally.
- Early (Active) Stages: Variable enhancement after intravenous contrast.
- Late (Inactive) Stages: No enhancement.
Given the nonspecific imaging findings, percutaneous biopsy is often necessary to confirm the diagnosis and to exclude malignancy as an underlying cause.
XIII. Extramedullary Hematopoiesis [1, 14, 15]
Extramedullary hematopoiesis refers to blood cell formation occurring outside the bone marrow, often as a response to chronic anemia, leukemia, lymphoma, or other myeloproliferative disorders. Commonly involved sites include the liver, spleen, and paravertebral soft tissues.
- CT findings:
- Multiple bilateral homogeneous masses with soft tissue attenuation.
- Variable enhancement after contrast administration.