
1. Rectal Anatomy on MRI
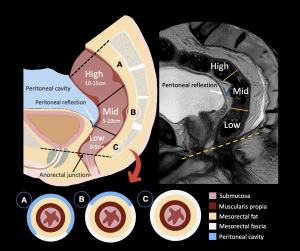
The rectum is divided according to its distance from the anorectal junction into low (0–5 cm), mid (5–10 cm), and high (10–15 cm).
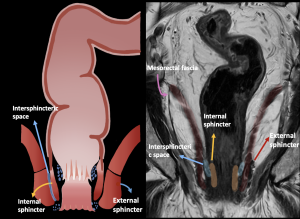
MRI depicts the rectal wall layers, the surrounding tissues and the sphincter complex, all of which are critical landmarks for staging and surgical planning.
2. MRI Tumor Staging
T Stage
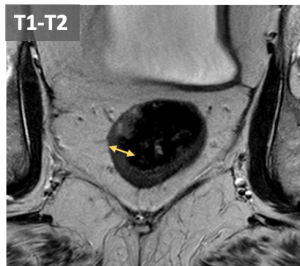
Differences in T2w signal intensity of the rectal wall layers allow accurate assessment of mural invasion and regional spread. The mucosa and muscularis propia appears hypointense while the submucosa is hyperintense.
- T1-T2: Preservation of the hypointense muscularis propia indicates tumor confined to the wall. Differentiation of T1 or T2 is not possible without submucosal edema.
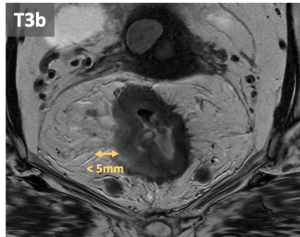
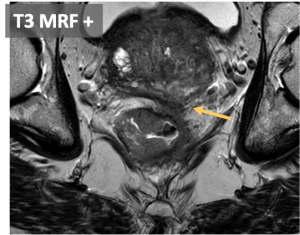
- T3: Tumor extension into the mesorectal fat, beyond muscularis propia. T3 can be subclassified according to the extramural invasion depth:
- T3a: <1 mm
- T3b: 1-5 mm
- T3c: 5-15 mm
- T3d: >15 mmm.
- Involvement of the mesorectal fascia (MRF+) is a associated with higher risk of local recurrence.
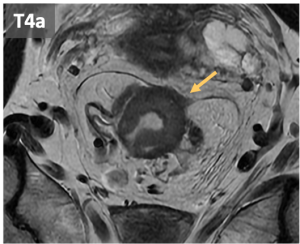
- T4: can be classified in:
- T4a: invasión of adjacent organs
-
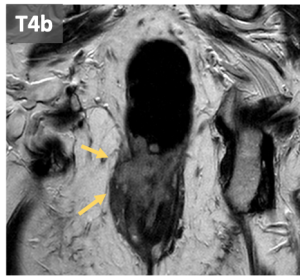
- T4b: invasion or pelvic organs including: pelvic organs, vascular structures outside the mesorectum, fat outside the mesorectum, small or large bowel in the pelvis, excretory system (ureters and urethra), muscle (external anal sphincter, puborectalis, levator ani, obturator, piriformis and ischioccygeus), sciatic or sacral nerves, ligaments (sacrosìnous /sacrotuberous), bone.
N stage
Regional lymph nodes include mesorectal, internal iliac, obturator, superior rectal, and inferior mesenteric nodes.
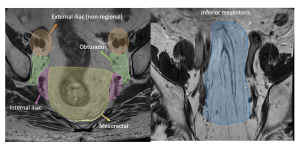
Non-regional nodes are considered metastasis and include external iliac, common iliac, inguinal, and retroperitoneal lymph nodes.
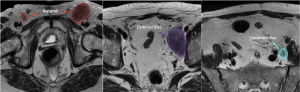
Malignant nodal features are round morphology, irregular margins, heterogeneous signal intensity, and size criteria. Mucinous lymph nodes are always suspicious.
Prognostic factors with higher risk of recurrence and metastasis:
- Extramural vascular invasion (EMVI): tumor sign into vascular structures.
- Anal sphincter and pelvic floor involvement: invasion of the external sphincter, puborectalis and elevator is considered a T4b whereas invasion of the internal sphincter does not change the staging.
- Tumor deposits within the mesorectal: irregular nodules situated within vessels. There is no criteria to discriminate them with lymph nodes.
3. Rectal cancer tumor staging
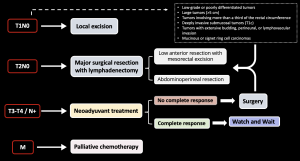
The managment of rectal cancer is guided by de TNM staging system which helps categorize patients into different risk groups and determine the most appropiate management for each group:
- Local or low risk disease (Stage 0 and I): Tumor confined to the rectal wall (T1 and T2) without lymph node involvement (N0) and without distant metastasis (M0).
- Locally advanced or intermediate risk disease (Stage II and III): Includes T3-T4 or any T stage with regional lymph node involvement (N1-N2). These patients typically needs neoadyuvant therapy to reduce tumor size and decrease local recurrence.
- Metastatic or high risk disease (Stage IV): Defined by the presence of distant metastasis.
Therapeutic pathways by stage
- T1N0: local excision. radical surgery is recommended in the presence of high risk features includig:
- Poorly differentiates histology
- Large tumor size (>5 cm) or involvemente of more than one-third of the rectal circumference
- Deep submucosal invasion
- Extensive tumor budding, perineural invasion or lymphovascular invasion
- Mucinous or signet ring cell carcinoma
- T2N0: Major surgical resection with lymphadenectomy, most commonly low anterior resection with total mesorectal excision or abdominoperineal resection depending on the rectal localization of the tumor.
- T3-T4 and/ or N+ disease: Neoadjuvant therapy followed by imaging postneoadyuvant evaluation:
- Complete response: watch-and-wait organ-preservation strategy
- Incomplete response: surgical resection
- M+: Treatment consist of systemic palliative chemotherapy.
Reevaluation of patients with neoadyuvant therapy
Multidisciplinary re-evaluation determines if the patient is candidate for organ-preserving strategies. This assessment is performed at scheduled intervals (starting at 12 weeks) using a combination of MRI, endoscopy, and clinical examination with digital rectal exam.
- Complete response: Watch and wait strategy, avoiding the morbidity of radical surgery.
- Adequate / partial response: May requiere a secondary assesment 4 weeks later to determine if the patient can avoid radical surgery.
- Poor response: Total Mesorectal Excision (TME)
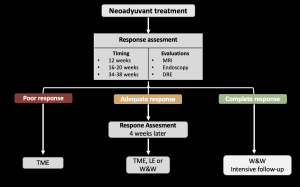
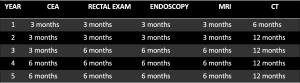
Watch and Wait strategy
Patients with a complete radiological response can be individually evaluated to implement an organ-sparing strategy (watch and wait) if there is also a complete response in endoscopic and digital rectal exams.
This strategy requires close follow-up which includes:
- Clinical examination with digital rectal exam
- Endoscopy
- High-resolution pelvic MRI
- Analysis with markers (CEA)
4. MRI protocol
- Scout in all 3 planes
- TSE T2 sagittal FOV pelvis; 3/0.3mm thickness. Include sacral promontory. Used as reference to angle the rest of the sequences
- TSE T2 axial pelvis (including promontory); 3/0.3 mm slice thickness
- TSE T2 axial oblique to the tumor; 3/0.3 mm slice thickness. Oriented with the short axis of the tumor/affected rectal segment.
- TSE T2 coronal oblique to the tumor; 3/0.3 mm slice thickness. Oriented with the long axis of the tumor/affected rectal segment (perpendicular to the previous)
- DWI axial oblique to the tumor. Oriented with the short axis of the tumor/affected rectal segment
- T2 coronal oblique to the anal canal; 3/0.3 mm slice thickness
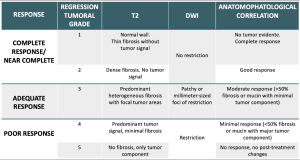
5. Neoadjuvant Treatment and MRI Response Assessment
Patients with locally advanced rectal cancer typically undergo neoadjuvant chemoradiotherapy followed by surgical resection. In selected patients with complete clinical and radiological response, watch-and-wait strategy may be considered.
MRI reassessment is usually performed 6–12 weeks after neoadyuvant treatment. Expected post-treatment changes of the primary tumor includes:
- Decrease in tumor volume and extension,
- Development of low-signal fibrosis on T2-weighted images,
- Normalization of layered structure of the wall.
The tumor response is classified by MR in complete response, adequate response and poor response.
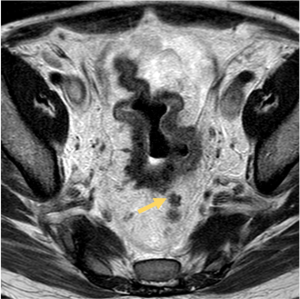
The imaging criteria for recurrence after complete response include:
- Increase in fibrotic scar depth angle >21°.
- Thickening of the fibrotic scar >10 mm (first sign of suspicion)
- New nodular areas with heterogeneous or intermediate T2 signal or diffusion restriction.

6. Common pitfalls in MRI restaging
- Persistent high T2 signal in mucinous tumors, with or without tumoral cells
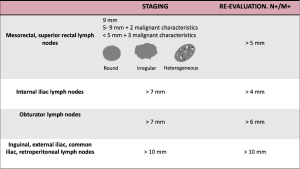
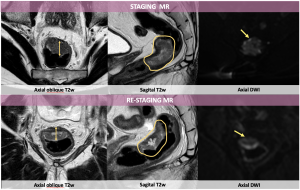
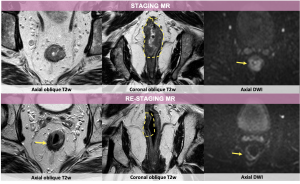
 Fig 21: Staging MR demonstrates a concentric mural thickening of the lower and middle rectum with a high T2 signal component, suggestive of a mucinous tumor. Post-neoadyuvance evaluation MR shows persistent high-signal thickening with no residual tumor in the histological analysis after surgery.
Fig 21: Staging MR demonstrates a concentric mural thickening of the lower and middle rectum with a high T2 signal component, suggestive of a mucinous tumor. Post-neoadyuvance evaluation MR shows persistent high-signal thickening with no residual tumor in the histological analysis after surgery. - Mucin pools development in nonmucinous adenocarcinoma because of colloid degeneration, with or without tumoral cells.
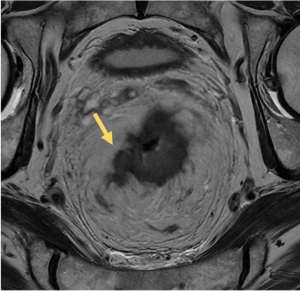
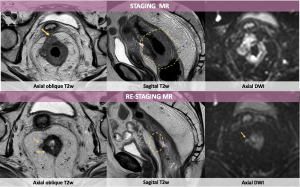
 Fig 22: Pitfall: Colloid degeneration of nonmucinous adenocarcinoma after treatment, with or without tumoral cells. Axial MR of the mid rectum which shows (A) intermediate T2 mural thickening and (B) New high signal intensity after neoadjuvant treatment due to mucin pool/colloid degeneration.
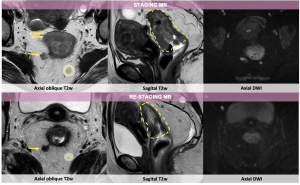
Fig 22: Pitfall: Colloid degeneration of nonmucinous adenocarcinoma after treatment, with or without tumoral cells. Axial MR of the mid rectum which shows (A) intermediate T2 mural thickening and (B) New high signal intensity after neoadjuvant treatment due to mucin pool/colloid degeneration. - Submucosal edema due to neoadyuvant treatment, often misinterpreted as residual tumor.
- Diffusion-weighted imaging artifacts (T2 shine-through and T2 dark-through)
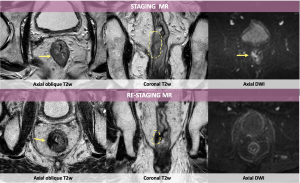
 Fig 23: Illustration of the different types of diffusion weighted imaging (DWI) pitfalls.
Fig 23: Illustration of the different types of diffusion weighted imaging (DWI) pitfalls. - Signal alterations related to intraluminal contents. In these cases, tumor recurrence should be suspected if the shape of the signal increase is curvilinear or in the shape of a C or U, similar to a mass. If the morphology is star-shaped, it suggests content.
7. Proposed structured report
PROTOCOL: Overall study quality: Adequate/Suboptimal/Non-diagnostic: Reason.
PRIOR MRI: Yes/No Date and staging:
LOCALIZATION AND CHARACTERISTICS OF THE LESION:
- Low rectum (0-5 cm) / medium (5-10 cm) / high (10-15 cm).
- Lesion length: Distance from the most distal end of the tumor to the anal margin = cm.
- Distance from the most distal end of the tumor to the sphincter complex = cm.
- Tumor relationship with the peritoneal reflection.
RE-EVALUATION AFTER NEOADJUVANT CHEMORADIOTHERAPY:
- No response
- Inadequate poor response with regression reduction less than 25%. Small areas of fibrosis or mucin.
- Adequate incomplete/poorly moderate response: > 50% fibrosis or mucin and 50% of tumor foci visible.
- Adequate practically/possibly complete (assess new MRI in 4 weeks) Dense fibrosis, minimal tumor. Reduction >75% with fibrosis.
- Complete radiological response. No evidence of the previous presence of tumor. Only fibrosis (100%).
- yrmCRM: No change/probable negativization/positivization.
- yrmTRG IVEM (no change/negativization/positivization)
- Re-staging of categories T and N if applicable (yrmTNM):
CONCLUSION/EVALUATION OF RESPONSE:
- Almost complete-complete: normalization of rectal wall or only fibrosis.
- Good response/adequate: predominance of fibrosis, but with residual tumor component in pT2 or in DWI.
- Poor response/poor/inadequate: predominant tumor component
ADDITIONAL COMMENTS: