Definition
The term ectopic varices refers to any large portosystemic collaterals occurring outside the gastroesophageal region, including portosystemic shunts, gastric varices outside the cardia, rectal varices, internal hemorrhoids, and nongastrointestinal varices [1,3].
Although their true prevalence and distribution remain uncertain due to their rarity, ectopic varices present a significant clinical challenge that requires a multidisciplinary approach, with interventional radiology playing an increasingly vital role [1]. A Japanese national survey [2] highlights a discrepancy between endoscopically diagnosed and interventionally treated ectopic varices, suggesting that endoscopy may be effective for managing rectal and duodenal varices, while interventional radiology is better suited for other locations [1].
The mortality rate from recurrent bleeding can reach up to 40% [1].
Ectopic varices secondary to portal hypertension develop natural portosystemic shunts [3]. While healthy subjects maintain low resistance in the portal venous system and high resistance in these collaterals, intrahepatic portal hypertension redirects blood through these shunts to bypass increased hepatic vascular resistance. Surgical literature and cadaver studies have identified portosystemic connections through: (a) the gastroesophageal plexus to the azygous-coronary system, (b) the hemorrhoidal plexus, (c) recanalized umbilical vein, (d) the pancreatoduodenal venous arcade to the inferior vena cava via retroperitoneal veins of Retzius, (e) splenorenal, and (f) mesogonadal shunts [3]. In Western countries, most cases of ectopic variceal bleeding are associated with intrahepatic portal hypertension [3].
Anatomic locations and clinical presentations
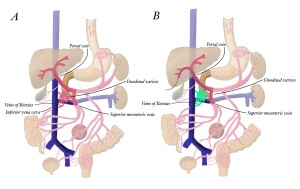
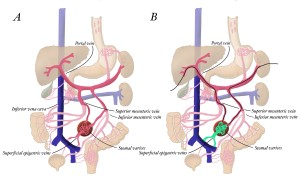
Figure 1 illustrates the vascular anatomy of various types of ectopic varices encountered in clinical practice. Each variant requires a tailored approach based on its unique anatomical and hemodynamic features. The clinical manifestations depend on the location of the varices.

Rectal varices (Figure 2) are the most common type, with blood supply derived from the inferior mesenteric vein, draining through the middle and inferior rectal veins into the internal iliac veins. They typically present with hematochezia [1].

Duodenal varices (Figure 5) have a distinctive vascular pattern where the feeding vessels originate from mesenteric veins, specifically branches from the portal or superior mesenteric vein. Their drainage follows the Retzius vein system to the inferior vena cava. They usually manifest as hematemesis or melena [1].
Stomal varices (Figure 7) are supplied by both superior and inferior mesenteric veins, draining through the superficial and inferior epigastric veins to the cavo-iliac venous system. They are readily identified through active bleeding at the stoma site [1].
Other less common sites include varices in the biliary tract, which may cause biliar obstruction, hemobilia or gastrointestinal hemorrhage; varices in the urinary bladder, which can result in hematuria; varices at the right hemidiaphragm which may result in hemothorax; abdominal wall varices, such as umbilical varices, can rupture and cause internal or external bleeding; and varices at the falciform ligament, diaphragm, splenic ligament or rectovesical region pose a significant risk of intraperitoneal rupture [3].