Ovarian Vein Thrombosis in a Postmenopausal Woman (fig. 1)
IntroductionOvarian vein thrombosis (OVT) is a rare but potentially life-threatening condition, most associated with postpartum status or hypercoagulable states. In postmenopausal women, OVT is exceptionally rare and often misdiagnosed due to its nonspecific presentation, mimicking nephrolithiasis or pyelonephritis. Given its potential complications, including pulmonary embolism and sepsis, early imaging-based diagnosis is essential.
Case PresentationA 72-year-old postmenopausal woman presented with a one-week history of left-sided colicky flank pain. The pain was sharp, intermittent, and non-radiating, with no urinary or gastrointestinal symptoms. On examination, she had a low-grade fever (38.2°C) and mild tenderness in the left lower quadrant.
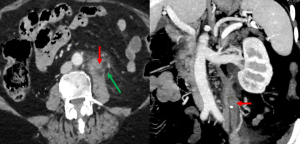
CT Findings
- Tubular structure in the left ovarian vein with an enhancing wall and central low-attenuation thrombus
- Perivascular fat stranding, suggesting inflammation
- Ipsilateral ovarian enlargement, consistent with venous congestion
These findings confirmed the diagnosis of left-sided OVT, a rare occurrence in postmenopausal women.
ConclusionThis case highlights the importance of CT imaging in diagnosing atypical OVT presentations. In postmenopausal women with unexplained flank or abdominal pain, OVT should be considered in the differential diagnosis, and early anticoagulation therapy is critical to prevent thromboembolic complications.
Abdominal Fat Necrosis:
Fat necrosis in the abdomen can mimic acute surgical conditions, often resulting from ischemia, inflammation, or trauma affecting adipose tissue. Common locations include the greater omentum, mesentery, and falciform ligament. Differentiating these conditions through imaging is crucial for appropriate management.
Case 1: Falciform Ligament Fat Necrosis with Abscess Formation (fig. 2)

Case PresentationA 54-year-old woman presented with acute epigastric pain. Examination revealed mild upper abdominal tenderness without peritoneal signs. Laboratory findings were normal except for a mild leukocytosis.
CT Findings
- Heterogeneous fat density with a hyperattenuating peripheral rim near the falciform ligament
- Enlargement of the falciform ligament with a localized fluid collection
- Hepatic parenchymal enhancement surrounding the collection, suggesting an evolving abscess
These findings were consistent with falciform ligament fat necrosis complicated by abscess formation. The patient was treated with antibiotics and percutaneous drainage, resulting in improvement.
DiscussionThe falciform ligament is a peritoneal fold that divides the right and left subphrenic spaces, containing paraumbilical veins, ligamentum teres, and fatty tissue. Necrosis is extremely rare and often misdiagnosed, mimicking cholecystitis, perforated ulcer, or pancreatitis. The primary causes include infection, torsion, venous thrombosis, or embolism.
Imaging Considerations
- Ultrasound may show an oval hyperechoic mass with a hypoechoic halo.
- CT scan is the gold standard, revealing a non-enhancing fatty lesion with inflammatory stranding and fluid collection.
Early imaging recognition is crucial to prevent complications like abscess formation, which may require surgical or percutaneous intervention. In uncomplicated cases, supportive care with antibiotics is the preferred approach.
Case 2: Omental Infarction Presenting as an Isolated Fat Lesion (fig. 3)

Case PresentationA 36-year-old man presented with acute right lower quadrant pain. He denied trauma, surgery, or strenuous activity.
CT Findings
- Encapsulated fat lesion in the greater omentum, without contrast enhancement
- Surrounding inflammatory fat stranding, characteristic of ischemia
- No adjacent bowel involvement, ruling out alternative diagnoses
These imaging features were consistent with primary omental infarction, likely due to spontaneous vascular compromise. The patient was managed conservatively with analgesia, and symptoms resolved.
DiscussionThe greater omentum is a highly vascular peritoneal fold that functions as a protective barrier. Omental infarction is rare due to its extensive collateral circulation, but the right lateral free edge is particularly vulnerable due to its weaker blood supply.
Mechanisms of Omental Infarction: (see table)
CT Features of Omental Infarction:
- Fatty encapsulated mass (>5 cm) with soft-tissue stranding
- Early infarction: Mild fat haziness
- Omental torsion: May show swirling vessels
- Complications: Can progress to infection or abscess formation
Diagnosis is radiologic, with CT scans playing a central role in differentiation from appendicitis or cholecystitis. Management is conservative, unless complications arise.
Cecal Volvulus (fig. 4)

Cecal volvulus, a rare cause of acute large bowel obstruction. This condition occurs when the cecum abnormally twists or folds, leading to intestinal obstruction and potential ischemia. Early recognition through CT imaging is essential for timely intervention and to prevent complications such as perforation or necrosis.
Case Presentation: Cecal Volvulus (Cecal Bascule)
A 67-year-old woman with a history of chronic constipation and prior abdominal surgery presented with progressive abdominal distension and cramping pain over the past 24 hours. On examination, she had a distended, tympanic abdomen with mild tenderness in the lower quadrants. Bowel sounds were present but reduced.
CT Findings:Abdominal CT (coronal and axial views) revealed:
- Distended cecum folded over itself without evidence of torsion.
- "Whirl sign” spiraled loops of the collapsed cecum and twisted mesentery.
- Superior displacement of the appendix (red arrow) and terminal ileal loop.
- No signs of small bowel obstruction or ischemia.
Findings were consistent with cecal bascule, a subtype of cecal volvulus where the cecum folds anteriorly without torsion.
Discussion
Cecal volvulus results from abnormal mobility of the cecum, leading to bowel obstruction. It occurs in two forms:
- Axial torsion: The cecum rotates around its axis, leading to whirl and bird beak signs on CT.
- Cecal bascule: The cecum folds forward without twisting, often seen as a dilated loop in the mid-abdomen.
CT plays a key role in diagnosis, distinguishing between types and assessing complications like ischemia. Endoscopic decompression is the first-line treatment for cecal bascule, while surgical intervention (cecopexy or resection) is needed for recurrent or complicated cases.
Internal hernia: (fig. 5)

Internal hernias occur when abdominal viscera protrude through an abnormal opening within the peritoneal cavity. These defects can be congenital (due to incomplete peritoneal fusion) or acquired (secondary to trauma, inflammation, or surgery).
Case Presentation
A 58-year-old multiparous woman presented with acute abdominal pain, nausea, and bloating. The pain was localized to the lower abdomen, with no history of prior surgery. On examination, abdominal distension and tenderness were noted, but there were no peritoneal signs.
CT Findings
- Dilated small bowel loops with a transition point in the pelvis.
- Entrapment of bowel lateral to the uterus, consistent with a broad ligament hernia
Discussion
Broad ligament hernia is a rare pelvic internal hernia where the bowel becomes trapped within or passes through a defect in the broad ligament. It occurs mostly in multiparous women and commonly involves the small intestine. Defects are classified into:
- Fenestra type – Herniation through both peritoneal layers, with no hernia sac.
- Pouch type – Herniation into one peritoneal layer, forming a sac.
CT diagnosis is critical, showing mesenteric vessels passing through the broad ligament and uterus-ovary displacement. Surgical repair is required to prevent ischemia and bowel strangulation.
Perforated Meckel’s Diverticulitis (fig. 6)

A 14-year-old boy presented with acute lower abdominal pain, worsening over 24 hours, accompanied by low-grade fever and nausea. Examination revealed tenderness in the right lower quadrant with mild guarding. Laboratory tests showed elevated inflammatory markers.
CT Findings
- Blind-ending fluid-filled structure in the distal ileum
- Mural thickening and surrounding fat stranding, consistent with inflammation
- Free air and localized fluid collection, indicating perforation
Discussion
Meckel’s diverticulum is a remnant of the vitelline duct, typically located 30–60 cm from the ileocecal valve. Complications arise from gastric acid secretion, leading to ulceration, obstruction, or perforation. CT is the preferred imaging modality, aiding in identifying complications such as Meckel’s diverticulitis, obstruction, intussusception, or Littre’s hernia (in which a Meckel’s diverticulum becomes incarcerated within a hernial sac).
Pelvic Actinomycosis (fig. 7)

A 42-year-old woman presented with chronic pelvic pain, low-grade fever, and intermittent vaginal discharge. On examination, she had lower abdominal tenderness without peritoneal signs.
CT Findings
- Complex intrauterine fluid collection, suggesting infection
- Marked thickening and enhancement of the sigmoid colon wall
- Surrounding pelvic fat stranding, indicative of inflammatory spread
Discussion
Pelvic actinomycosis is a rare, chronic bacterial infection, often linked to long-term IUD use. It can mimic pelvic inflammatory disease, tubo-ovarian abscess, or malignancy. The infection spreads aggressively, crossing fascial planes and involving surrounding organs such as the colon, bladder, and uterus. CT imaging reveals heterogeneous pelvic masses, abscesses, or bowel wall thickening. Unlike malignancies, regional lymphadenopathy is uncommon. Diagnosis requires microbiological or histopathological confirmation. Prolonged antibiotic therapy (penicillin-based) is the mainstay of treatment, with surgical intervention reserved for complications such as abscess rupture or obstruction.