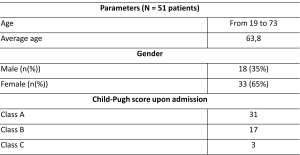
The study was conducted at the Department of Interventional Radiology at the University Medical Center. The study group included 51 patients hospitalized between February 2021 and September 2023. The patients' ages ranged from 19 to 73 years, with 18 men (35%) and 33 women (65%).
The primary criterion for patient selection was the presence of liver cirrhosis, portal hypertension, hypersplenism, and a history of variceal bleeding. The severity of liver cirrhosis was assessed using the Child-Pugh classification: Class A - 31 patients, Class B - 17 patients, and Class C - 3 patients. All patients had intrahepatic block portal hypertension, meaning liver cirrhosis developed as a result of viral hepatitis.
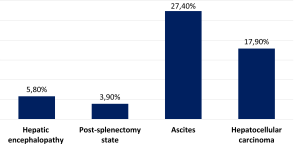
In the medical history, episodes of bleeding from esophageal and gastric varices, combined with hypersplenism, were observed in all patients. Hepatic encephalopathy was present in 3 patients (5.8%), 2 patients (3.9%) had undergone splenectomy, 14 patients (27.4%) had ascites, and 9 patients (17.9%) had hepatocellular carcinoma.
A total of 70 surgical interventions were performed: 3 transjugular intrahepatic portosystemic shunt (TIPS) procedures (4.2%), 29 splenic artery embolizations (SAE) (41.4%), and 38 embolizations of gastric and esophageal varices (54.1%).
Endovascular interventions were performed in X-ray operating rooms equipped with angiographic units.