Diverticular disease includes two main conditions: diverticulosis and diverticulitis. Diverticulosis is the presence of one or more intestinal outpouchings, called diverticula, in the colon or small intestine. Colonic pseudodiverticula, or false diverticula, form when mucosa and submucosa herniate through the muscular layer at sites where blood vessels enter the colon, a phenomenon most commonly observed in the sigmoid colon [1], [2].
The prevalence of diverticular disease has increased over the past century and has traditionally been regarded as a condition primarily affecting Western countries, due to an increased prevalence of a low-fiber diet: this disease is most common in the United States, Europe, and Australia, where approximately 50% of people >60 years old are affected by diverticulosis [3].
When inflamed, colonic diverticula cause ACD, the most common complication of diverticular disease. Clinical presentation is typically adequate for an accurate diagnosis: patients with symptomatic diverticular disease commonly report vague abdominal discomfort, along with tenderness, bloating, and changes in bowel habits, such as constipation or diarrhea. Furthermore, individuals with acute diverticulitis may experience symptoms like nausea, vomiting, fever, elevated white blood cell count, and occasionally urinary issues. The manifestation of diverticulitis is influenced by factors such as the location of the affected diverticulum, the degree of inflammation, the duration of the infection, and any complications, ranging from localized inflammation to life-threatening fecal peritonitis.

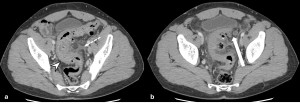
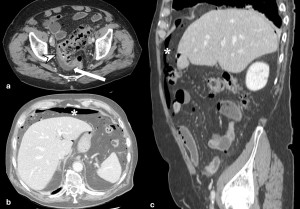
Radiological confirmation is often required for the diagnosis of ACD. Abdominal contrast enhanced CT (CE-CT) is considered the gold standard for diagnosing diverticulitis, as well as for distinguishing between uncomplicated and complicated forms of the condition [5]. In CT scans of acute colonic diverticulitis, findings can be broadly classified into two groups: those related to the bowel wall, which highlight the inflamed diverticulum itself, and extra-intestinal findings, which may indicate the extension of inflammation and the presence of complications [4].
Based on the presence or absence of these findings, it is possible to stage the severity of the condition. The most widely used staging system is the Hinchey surgical classification, which was updated in 2005 to incorporate specific CT findings. This system includes six stages of escalating severity, ranging from 0 to 4, with sub-stages 1a and 1b [6], [7]. Another valuable staging system is the one introduced by the World Society of Emergency Surgery (WSES) in 2020, which features seven stages of escalating severity, including additional sub-stages 2a and 2b [8].
In cases of acute diverticulitis, alterations of certain parameters in haematochemical tests may be observed. For example, the evaluation of white blood cells (WBCs) has long been a fundamental aspect in diagnosing diverticular disease. An elevated WBC count is regarded as one of the primary clinical indicators for diagnosing acute diverticulitis, particularly when accompanied by left lower quadrant pain and abdominal tenderness [9]. Another commonly evaluated marker is CRP. This protein is synthesized in the liver as an acute-phase reactant in response to cytokines released at the site of inflammation. In response to an acute-phase trigger, CRP production is swiftly increased. As a key acute-phase reactant, CRP levels are elevated in acute diverticulitis and are considered one of the most effective biomarkers for this condition [5], [10].
Therefore, several recent studies have explored the potential link between laboratory findings and acute diverticulitis, aiming to establish cut-off values and showing that both WBC and CRP may serve as predictors of the condition's severity [11].
Recently, there has been growing interest in utilizing certain "new" laboratory parameters to predict the severity of a diverticulitis episode, helping to determine whether conservative or surgical treatment is more appropriate. The LNR and the platelet-to-lymphocyte ratio (PLR) have demonstrated promising potential for these purposes [12], [13].
The study was conducted at the Radiology Department 1 of the University Hospital ‘G. Rodolico-San Marco’ in Catania. We retrospectively evaluated a total of 131 patients diagnosed with acute diverticulitis by CT examination from 1 January 2021 to 31 August 2024. For each patient, we collected: biographical data such as sex and age at the onset of the episode; laboratory data of inflammatory biomarkers such as CRP, neutrophils and lymphocytes counts (and relative NLR) taken from the haematochemical tests performed on admission to the emergency department; the type of treatment received after diagnosis, i.e. whether conservative or surgical, and the corresponding hospitalization.
The severity of the condition was therefore assessed using the WSES and modified-Hinchey classification systems, based on the initial CT scans performed for each patient. The patients were categorized into three distinct groups based on the severity of their condition: low, moderate, and high severity, according to both the WSES (stage 0 patients included in the low group; patients 1a, 1b and 2a in the moderate group; patients 2b, 3, 4 in the high group) and modified-Hinchey (stage 0 and 1a patients included in the low group; patients 1b and 2 in the moderate group; patients 3 and 4 in the high group) classification systems.
In addition, two groups were created according to patients’ outcome: “clinical success” and “clinical failure”.
We assessed the relationship between inflammatory biomarkers and the severity of acute diverticulitis through ANOVA test; Spearman's rank correlation was performed. The correlation between inflammatory biomarkers and hospitalization time was assessed by Pearson’s correlation.
Moreover, the “clinical success” and “clinical failure” groups were compared with the laboratory tests (NLR and CRP) using the Mann-Whitney test.
Patients were further divided according to conservative or surgical treatment and the Mann-Whitney test compared the values of CRP and NLR between the two WSES and modified-Hinchey groups.
A statistical significance level of p<0.05 has been used for all tests.