ANATOMY
CLINICAL ANATOMY AND INNERVATION

The median nerve is a mixed motor and sensory nerve of the upper extremity, arising from the medial and lateral cords of the brachial plexus, receiving contributions from the C5-T1 nerve roots. Understanding the nerve course and its innervation is imperative for identifying potential entrapment sites and their clinical implications.
Arm: In the arm, the median nerve traverses between the biceps brachii and brachialis adjacent to the brachial artery. There are no major branches from the median nerve in the arm.
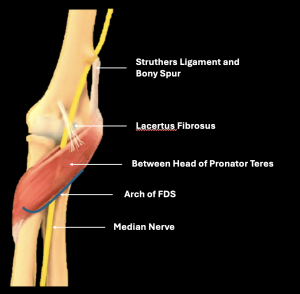
Elbow and Forearm: The median nerve then enters the cubital fossa and courses beneath the bicipital aponeurosis, aka lacertus fibrosus, medial to the brachial vessels. In the proximal forearm, it passes between the humeral and ulnar heads of the pronator teres (PT), forming the pronator tunnel. After exiting the pronator teres, it then enters under the flexor digitorum superficialis (FDS) fibrous arch, aka the sublimis bridge. It then traverses between the flexor digitorum superficialis (FDS) and flexor digitorum profundus (FDP) musculature [3-5].
Motor branches to the pronator teres, palmaris longus, Flexor Digitorum Superficialis (FDS), and Flexor Carpi Radialis (FCR) arise from the main trunk at the level of the elbow and proximal forearm. The Anterior Interosseous Nerve (AIN) is a purely motor branch that originates at the level of the pronator teres. It runs superficial to the interosseous membrane along the anterior interosseous artery and supplies the radial half of Flexor Digitorum Profundus (FDP), Flexor Pollicis longus (FPL), and pronator quadratus. The palmar cutaneous branch (PCB)arises a few centimetres proximal to the wrist crease and is a sensory branch to the thenar area. It is classically spared in carpal tunnel syndrome due to its proximal origin [1].
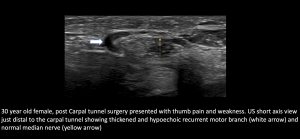
Wrist: At the wrist, the median nerve emerges along the lateral aspect of FDS and becomes more superficial, running deep to the palmaris longus towards the carpal tunnel. The median nerve lies superficially within the carpal tunnel, just deep to the flexor retinaculum, aka the transverse carpal ligament. The main trunk here terminates into a recurrent motor branch, which supplies the thenar group of muscles, and the common palmar digital branches, which provide sensory supply to the volar surface and finger tips of the 1st-3rd digits, and to the radial aspect of the 4th digit, as well as motor supply to the first two lumbricals [3].
POTENTIAL NERVE ENTRAPMENT SITES (BEYOND THE CARPAL TUNNEL)
The nerve is susceptible to compression during its course through anatomical narrow spaces, such as fibro-osseous/fibromuscular tunnels, the intramuscular course, and accessory ligaments and muscles.
The potential sites of proximal nerve compression along its usual anatomical course include under the lacertus fibrosus, along the pronator tunnel, and under the FDS arch, which are illustrated
Other potential causes of extrinsic compression include bicipitoradial bursitis, ganglion cysts, tumours, post-traumatic or post-operative scars, and foreign bodies.
Sometimes anatomical variants can predispose the nerve to compression. One such variant is the Struther’s ligament, which connects the supracondylar spur to the medial epicondyle. Neurovascular bundles, including the median nerve, can be compressed along their course adjacent to the spur or the ligament. Even accessory muscles are known to cause median nerve entrapment in the forearm. One such example is the Gantzer muscle, an anomalous head of the FPL [1,3,5].
NORMAL ULTRASOUND FINDINGS
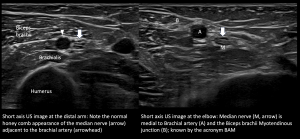
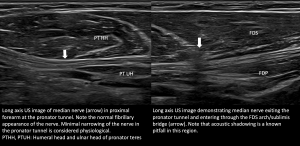
The median nerve appears round to ovoid in the short axis plane with hypoechoic internal fascicles against a background of hyperechoic interfascicular epineurium, which in turn is surrounded by an external echogenic epineurium giving it a honeycomb appearance. In the long axis, the nerve has a fibrillary pattern. No increased vascularity is demonstrated on the Doppler study [3,5].
Although cut-offs for cross-sectional area at the carpal tunnel are well established, there is insufficient dedicated literature for these cut-offs at other sites. Comparison with the normal opposite site can be helpful when in doubt. The nerve fascicles are usually more prominent in the arm and become smaller distal to the elbow [5].
Dynamic assessment with stress manoeuvres like pronation- supination and flexion-extension, or using targeted probe pressure to elicit symptoms (Sonographic Tinel’s), can be further helpful in localising the site of involvement [6].
PATHOLOGY
CLINICAL PRESENTATION:
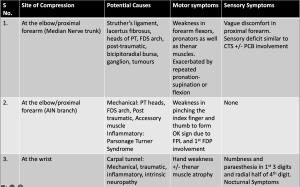
Clinical manifestations of median nerve pathologies depend on the site of involvement; however, they can overlap. The common pathologies and their manifestations are tabulated in [
ULTRASOUND FINDINGS IN PERIPHERAL NEUROPATHY:
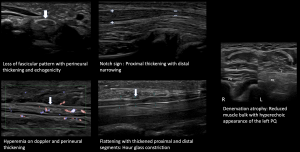
Nerve pathology can present with a variety of imaging appearances, depending on the degree and pattern of injury [7]. Common US findings in peripheral nerve pathology include nerve thickening, loss of fascicular appearance, perineural thickening, hyperemia, notch sign, hourglass constriction, and denervation of muscle groups, as demonstrated in
CASE SPECTRUM WITH IMAGING FINDINGS:
Clinical presentation and US findings of cases involving pathologies of the median nerve and its branches outside the carpal tunnel have been illustrated. The cases listed below are described in the respective figures.
1.Entrapment Neuropathies at Proximal Forearm:
- Compression under Lacertus Fibrosus
 Fig 7: COMPRESSION UNDER LACERTUS FIBROSUS
Fig 7: COMPRESSION UNDER LACERTUS FIBROSUS - Compression at Pronator Tunnel
 Fig 8: COMPRESSION AT THE PRONATOR TUNNEL
Fig 8: COMPRESSION AT THE PRONATOR TUNNEL - Compression at Flexor Digitorum Superficialis (FDS) Arch
 Fig 9: COMPRESSION UNDER FDS ARCH
Fig 9: COMPRESSION UNDER FDS ARCH - Charcot Marie Tooth Disease with superimposed Bilateral Double Crush Syndrome: Compression at Pronator Tunnel and Carpal Tunnel
 Fig 10: CHARCOT MARIE TOOTH DISEASE WITH SUPERIMPOSED COMPRESSION AT TWO SITES (DOUBLE CRUSH SYNDROME) Nerve thickening due to underlying hereditary neuropathy
Fig 10: CHARCOT MARIE TOOTH DISEASE WITH SUPERIMPOSED COMPRESSION AT TWO SITES (DOUBLE CRUSH SYNDROME) Nerve thickening due to underlying hereditary neuropathy Fig 11: CHARCOT MARIE TOOTH DISEASE WITH SUPERIMPOSED COMPRESSION AT TWO SITES (DOUBLE CRUSH SYNDROME) Compression of Right Median Nerve at the Pronator Tunnel
Fig 11: CHARCOT MARIE TOOTH DISEASE WITH SUPERIMPOSED COMPRESSION AT TWO SITES (DOUBLE CRUSH SYNDROME) Compression of Right Median Nerve at the Pronator Tunnel Fig 12: CHARCOT MARIE TOOTH DISEASE WITH SUPERIMPOSED COMPRESSION AT TWO SITES (B/L DOUBLE CRUSH SYNDROME) Compression of Right Median Nerve at the Carpal Tunnel
Fig 12: CHARCOT MARIE TOOTH DISEASE WITH SUPERIMPOSED COMPRESSION AT TWO SITES (B/L DOUBLE CRUSH SYNDROME) Compression of Right Median Nerve at the Carpal Tunnel Fig 13: CHARCOT MARIE TOOTH DISEASE WITH SUPERIMPOSED COMPRESSION AT TWO SITES (DOUBLE CRUSH SYNDROME) Compression of Left Median Nerve at the Pronator and Carpal Tunnel
Fig 13: CHARCOT MARIE TOOTH DISEASE WITH SUPERIMPOSED COMPRESSION AT TWO SITES (DOUBLE CRUSH SYNDROME) Compression of Left Median Nerve at the Pronator and Carpal Tunnel
2.Post Surgical Causes of Nerve Pathology
- Post Carpal Tunnel Release (CTR) surgery, Palmar Cutaneous Branch (PCB) neuroma and Flexor Carpi Radialis (FCR) tenosynovitis
 Fig 14: POST CTR SURGERY PALMAR CUTANEOUS BRANCH (PCB) NEUROMA AND FCR TENOSYNOVITIS PCB neuroma and PCB hydrodissection with steroid injection
Fig 14: POST CTR SURGERY PALMAR CUTANEOUS BRANCH (PCB) NEUROMA AND FCR TENOSYNOVITIS PCB neuroma and PCB hydrodissection with steroid injection Fig 15: POST CTR SURGERY PALMAR CUTANEOUS BRANCH (PCB) NEUROMA AND FCR TENOSYNOVITIS Normal Median Nerve at Carpal tunnel; Persistent PCB neuroma
Fig 15: POST CTR SURGERY PALMAR CUTANEOUS BRANCH (PCB) NEUROMA AND FCR TENOSYNOVITIS Normal Median Nerve at Carpal tunnel; Persistent PCB neuroma Fig 16: POST CTR SURGERY PALMAR CUTANEOUS BRANCH (PCB) NEUROMA AND FCR TENOSYNOVITIS FCR tenosynovitis with tendinopathy
Fig 16: POST CTR SURGERY PALMAR CUTANEOUS BRANCH (PCB) NEUROMA AND FCR TENOSYNOVITIS FCR tenosynovitis with tendinopathy - Post Open Reduction Internal Fixation (ORIF)/Carpal Tunnel Release (CTR), median nerve neuroma/thickening at the wrist crease proximal to the carpal tunnel
 Fig 17: POST ORIF/CTR MEDIAN NERVE NEUROMA/THICKENING AT WRIST CREASE PROXIMAL TO THE CARPAL TUNNEL
Fig 17: POST ORIF/CTR MEDIAN NERVE NEUROMA/THICKENING AT WRIST CREASE PROXIMAL TO THE CARPAL TUNNEL Fig 18: POST ORIF/CTR MEDIAN NERVE NEUROMA / THICKENING AT WRIST CREASE PROXIMAL TO THE CARPAL TUNNEL Post ORIF hardware abutment and flexor tendinosis
Fig 18: POST ORIF/CTR MEDIAN NERVE NEUROMA / THICKENING AT WRIST CREASE PROXIMAL TO THE CARPAL TUNNEL Post ORIF hardware abutment and flexor tendinosis - Post coronary artery bypass graft surgery (CABG), Median Nerve Neuropathy in Mid Forearm
 Fig 19: POST SURGICAL(CABG) MEDIAN NERVE NEUROPATHY IN MID FOREARM
Fig 19: POST SURGICAL(CABG) MEDIAN NERVE NEUROPATHY IN MID FOREARM - Post ORIF Scar Entrapment, Median Neuropathy in Distal Forearm
 Fig 20: POST ORIF SCAR ENTRAPMENT MEDIAN NEUROPATHY
Fig 20: POST ORIF SCAR ENTRAPMENT MEDIAN NEUROPATHY
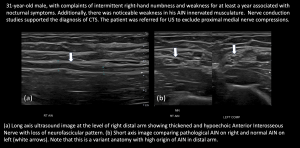
3.Anterior Interosseous Nerve (AIN) Pathology with pronator quadratus (PQ) atrophy
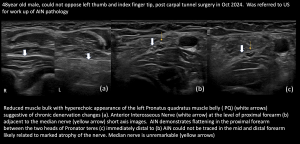
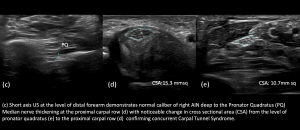
4.Anterior Interosseous Nerve with concurrent Carpal Tunnel Syndrome
5.Recurrent Median branch Pathology