Typical and atypical imaging features of IGM:
Ultrasound: Ultrasound findings are variable, ranging from a large hypoechoic mass to multiple clustered, often contiguous hypoechoic lesions with tubular extensions and with posterior acoustic shadowing[7]. According to a retrospective study involving over 200 patients, the most common ultrasound presentation of IGM is a large, irregular hypoechoic mass with tubular extensions (59%) [8]. Other ultrasound appearances include mass lesions with angular, lobulated, or indistinct margins; heterogeneous breast parenchyma; circumscribed hypoechoic masses; and parenchymal distortion with acoustic shadowing but without a discrete mass. In advanced disease, fluid collections or abscesses may be observed, with reported prevalences ranging from 6.6% to 54.0%. Ancillary ultrasound findings include skin thickening and edema, subcutaneous fat obliteration, and axillary adenopathy (characterized by smooth reactive cortical thickening with preserved fatty hilum), with reported frequencies varying widely[8].
Doppler ultrasound may demonstrate peripheral vascularity, generally without central vascularization. A contrast-enhanced ultrasound (CEUS) study showed that the prevalent BI-RADS score for IGM on standard ultrasound was 4, which decreased to BI-RADS 3 with the use of CEUS. CEUS findings of IGM frequently revealed peripheral enhancement (25%) compared to peripheral + central enhancement (5%), which contrasts with IBC, where central vascularity was observed in 31% of cases[9].
Mammography: Idiopathic granulomatous mastitis lacks specific mammographic features. It may appear normal or present as a mass with ill-defined or asymmetrical density, sometimes accompanied by skin thickening. In many cases, particularly in patients with heterogeneously or extremely dense breasts, IGM often does not show any notable mammographic findings (8–45%). Studies on IGM patients have identified focal asymmetry as the most common mammographic finding, with a reported prevalence of 36% to 75% [10]. Focal asymmetry refers to increased glandular tissue density visible on two projections (CC and MLO), involving less than one quadrant, without convex-outward borders, or interspersed with fat[11]. In more severe and extensive cases of the disease, mammography may reveal global asymmetry with pronounced skin thickening and trabeculation, which can be challenging to distinguish from IBC. Mass-forming IGM may appear as an irregular focal mass (11–67%) or, less commonly, as a circumscribed mass (9%), almost always without associated microcalcifications. Another rare mammographic manifestation of IGM is architectural distortion, reported in 9% of cases [8].
Magnetic Resonance Imaging: MRI findings of IGM are variable, similar to ultrasound and mammography, but MRI is significantly more sensitive than other imaging modalities. Despite the variability, T2 hyperintensity (indicative of edema) in the breast stroma is a common feature.
The most frequently observed MRI findings include heterogeneously enhancing masses or rim-enhancing lesions, often accompanied by associated segmental or regional non-mass enhancement (NME), with reported prevalence ranging from 71% to 86%. Some small lesions with well-defined borders, confluency, T2 hyperintensity, and rim enhancement are presumed to represent microabscesses. Less commonly (20%), IGM may present as a T2 hypointense mass with irregular borders [8]. Contrast enhancement in IGM exhibits variable kinetic properties, with the Type III washout pattern being rare. Most lesions demonstrate Type I kinetics (38.0–82.7%) or Type II kinetics (13.8–40.0%)[12].
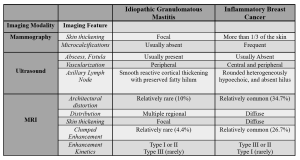
What radiological features differentiate idiopathic granulomatous mastitis from inflammatory breast cancer?
Most imaging findings of idiopathic granulomatous mastitis and inflammatory breast cancer can resemble each other, making differentiation challenging. On mammography, common features for both include asymmetric densities (focal and global), mass-forming lesions (irregular, spiculated), and axillary lymphadenopathy. Ultrasound may reveal similar findings, such as large hypoechoic masses or multiple clustered, often contiguous hypoechoic lesions with posterior acoustic shadowing and parenchymal distortion. MRI of IGM can also show features similar to IBC, including T2 hyperintensity (edema) of the breast stroma and prepectoral edema, which is considered highly suggestive of breast cancer. Additional shared features include rim-enhancing non-mass enhancement, mass-forming lesions with irregular borders, and changes in the skin and lymph nodes. While these overlapping features complicate differentiation, certain characteristics may favor one diagnosis over the other, as outlined in Table 1, which should also be supported by the patient's clinical feature.
Figures 1-2 represent cases of IGM, showcasing their mammography, ultrasound, and MRI findings.
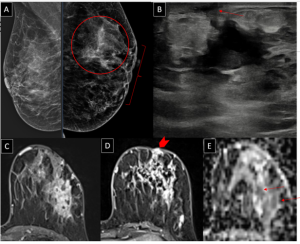
Figure 2 displays both pretreatment and post-treatment imaging results.
