- Acute physeal injuries:
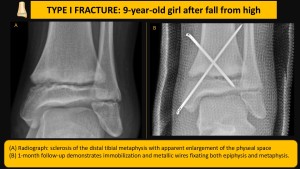
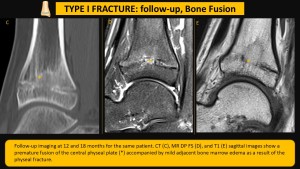
- Salter-Harris type I (Figures 2 and 3):
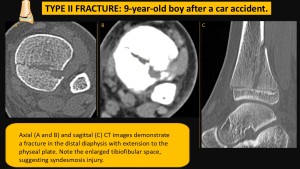
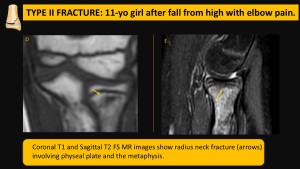
- Salter-Harris type II (Figures 4 and 5):
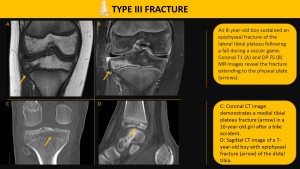
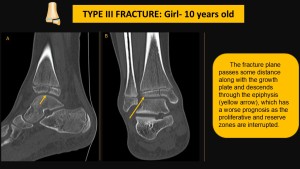
- Salter-Harris type III (Figures 6 and 7):
- Salter-Harris type IV (Figures 8 and 9):
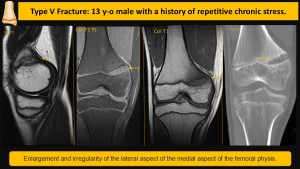
- Salter-Harris type V (Figure 10):
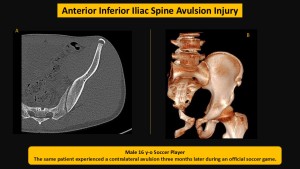
- Anterior Inferior Iliac Spine Avulsion Injury (Figures 11 and 12):
- Chronic Physeal Injuries (Figure 13):
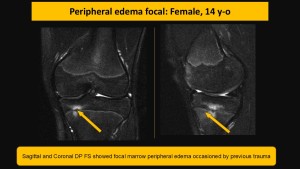
- Peripheral Edema Focal Areas (Figure 14):
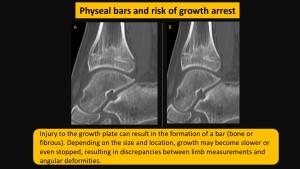
- Complications of Physeal Injuries (Figure 15):
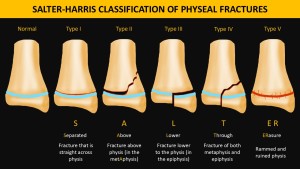
Fractures are relatively uncommon injuries that occur in children. Salter-Harris fractures (Figure 1) are injuries where a fracture of the metaphysis or epiphysis extends through the physeal. Not all fractures that extend to the growth plate are Salter-Harris fractures.
Salter-Harris type I fractures describes a fracture wholly contained within the physeal. There is no associated bone fragment. They must not involve epiphysis or metaphysis and must not have any rotated or angulated fragments.
In reality, the majority of fractures that involve the physeal have at least a small fragment of metaphysis associated with them and are, therefore, type II injuries.
The fracture must extend through the physis and into a part of the metaphysis. A triangular metaphyseal fragment, also known as the Thurston Holland fragment, will be left intact.
As stated before, most physeal fractures in children will be classified as type II Salter-Harris, corresponding to approximately 75% of them.
The most common site is the distal radius (circa 33-50%), followed by distal tibia, distal fibula, and phalanges.
Salter-Harris III fractures are rare intra-articular physeal fractures that occur in children.
The fracture line is often oriented obliquely through the epiphysis to the physeal, where it will have a horizontal orientation extending to the edge of the physeal. The fracture may also go through the epiphysis with a vertical/oblique orientation.
The prognosis of type III fractures can be poor if the reduction is not correct.
6.5-8% of physeal fractures will be Salter-Harris type III, seen most frequently in the distal tibia and distal phalanx.
Uncommon, intra-articular subtype in which the fracture extends through the epiphysis, physeal, and metaphysis.
They usually have a poor prognosis, and surgical intervention is often necessary.
10-12% of all physeal fractures will be Salter-Harris type IV fractures.
They most commonly involve the distal radius, phalanges, and distal tibia.
In the X-ray, the transparent fracture line extends through the metaphysis, the physeal, and the epiphysis.
Angulation, displacement, and rotation may occur adjacent to soft tissue edema, and joint effusion may be noted.
Computed Tomography can help better assess the nature of the fracture, evaluate the degree of displacement and anatomical extent of the fractures, and guide surgical intervention.
CT images can also be incorporated to assess the focal bone bridge through the physeal during the healing process (more common in Salter-Harris lesions IV and V).


Type V Salter-Harris fractures are rare, accounting for less than 1% of childhood fractures, and often occur due to compressive forces affecting the growth plate.
They typically have a poor prognosis as they can lead to vascular supply rupture, which may cause bone growth arrest and functional impairment. These fractures are frequently diagnosed retrospectively, as initial plain radiography often shows unremarkable results, although physeal narrowing may be observed.
Most cases remain hidden until clinical deformity or evidence of growth arrest emerges.
Additionally, soft-tissue edema and joint effusion are commonly present. CT imaging can be utilized during the healing phase to evaluate the formation of a focal bone bridge in the physeal area.
Pelvic apophyseal avulsion fractures are common in adolescents, particularly in males, and are often associated with kicking sports. These injuries typically occur due to forced hip extension while the knee is flexed. The straight head of the rectus femoris muscle originates from the anterior inferior iliac spine, and a forceful extension at the hip can lead to an avulsion at this site. In anteroposterior (AP) radiographs, the detached bone fragment may not always be visible; therefore, computed tomography (CT) and magnetic resonance imaging (MRI) can aid in diagnosis. It's important to recognize that subacute or chronic avulsion injuries can sometimes be mistaken for pseudotumors. Fortunately, most cases are managed conservatively.

Repetitive traumas, such as those encountered by elite teenage athletes, can lead to chronic damage to the body. Ongoing stress on the growth plate (physeal) can disrupt the blood vessels in the metaphysis, interfere with endochondral ossification, and cause the persistence of physical chondrocytes in the metaphyseal region.
Sports activities can specifically affect different joints; for example, physeal knee injuries are common among football and tennis players, while wrist injuries are prevalent among gymnasts.
Patients often experience chronic pain at the site of overuse injuries, and if the underlying stressor is not removed, the injury may progress.
This can lead to growth abnormalities and potential deformities.
MRI images of an affected growth plate typically appear enlarged and irregular, showing increased signal intensity on T2-weighted images
Early identification of these issues is crucial as it allows for appropriate rehabilitation and necessary modifications in activity patterns to prevent lasting consequences.

Focal areas of peripheral edema (FOPE) are often found incidentally during knee MRI evaluations in teenagers. These lesions appear as localized areas with decreased signal on T1-weighted images and increased signal on T2-weighted images, ranging from 2 mm to 3 cm, and show contrast enhancement. FOPE lesions typically manifest as edema near the closure of the growth plate (physeal) and may be linked to microtraumas from mechanical stress. The typical patient is a teenager, often aged 12 to 16, with a possible female predisposition. FOPE lesions are usually self-limiting and tend to resolve without treatment.
Injury to the growth plate can lead to the formation of a bar, which can be either bone or fibrous tissue. Depending on its size and location, this bar may slow growth or halt it altogether, resulting in discrepancies between limb lengths and angular deformities.
Radiography can reveal the presence of a bone bar as areas of osteocondensation that have a starry appearance or show bone structures at the interface between the metaphysis and epiphysis. Computed Tomography (CT) helps assess the interface between the metaphysis and the epiphysis, demonstrating the bone bars' location and size
Magnetic Resonance Imaging (MRI) is the most sensitive method for detecting these bars, particularly in cases involving non-ossified fibrovascularized bars.