Malignant Gastric Tumors
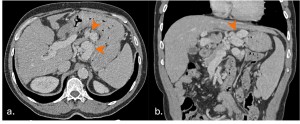
Gastric Adenocarcinoma
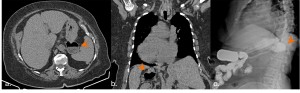
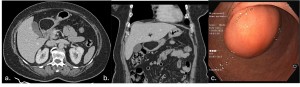
Adenocarcinoma accounts for 95% of all gastric cancers and typically presents as focal or segmental wall thickening (>1 cm) or as a discrete mass. The thickening may be asymmetric or circumferential, with irregular margins. Ulceration is common, and advanced cases may show perigastric fat infiltration, lymphadenopathy, or distant metastases [5, 6].
On contrast-enhanced CT, adenocarcinoma often shows heterogeneous enhancement in the arterial phase, with tumor staining in the venous phase. Mucinous adenocarcinoma may exhibit punctate or miliary calcifications within the tumor [3].
MDCT is highly accurate for staging, with a sensitivity > 90% for advanced carcinomas. However, early gastric cancers (limited to mucosa or submucosa) are more challenging to detect, with a sensitivity of 18% for depressed lesions [5].
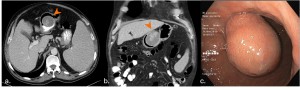
Gastric Lymphoma
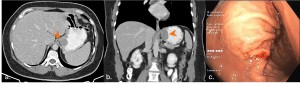
Gastric lymphoma represents 25% of extranodal lymphomas and is characterized by diffuse or segmental wall thickening (2-4 cm) with a significant lateral tumor extension. The thickening is usually homogeneous, but areas of low attenuation may be seen due to necrosis. Lymphadenopathy extending below the renal hila is a key feature [3].
Lymphoma tends to enhance less intensely than adenocarcinoma, with a more uniform appearance. Perigastric fat planes are often preserved, even in advanced cases [6].
CT can detect complications such as perforation, fistulization, or extragastric extension, which are more common in lymphoma than in adenocarcinoma [6].
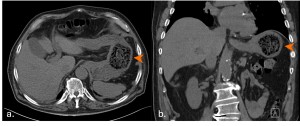
Gastrointestinal Stromal Tumors (GISTs)
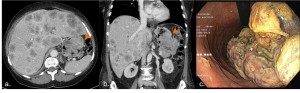
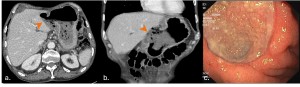
Gastrointestinal stromal tumors (GISTs) are common mesenchymal tumors typically found in the gastrointestinal tract, with the stomach being the most common site (60-70%)[3].
GISTs typically appear as well-defined, exophytic, and hypervascular masses that usually arise from the wall of the gastric body or antrum. Smaller tumors (<5 cm) are often intramural, whereas larger tumors (≥5 cm) may exhibit heterogeneous enhancement and commonly display central ulceration, necrosis, calcifications, and metastasis. [6, 7].
Features suggestive of malignancy include size >5 cm, irregular margins, and invasion of adjacent organs. However, definitive diagnosis requires histopathology [6].
Carcinoid Tumors
Gastric carcinoids are uncommon, accounting for only 0.3% of all gastric tumors. They are well-differentiated endocrine tumors with unique imaging characteristics and can be categorized into three subtypes, each with its own specific pathophysiological mechanism [3, 6].
On CT scans, Type 1 and 2 carcinoids appear as small, polypoid lesions in the gastric body and fundus. They are iso-dense in the pre-contrast phase but show marked enhancement during the arterial phase. Type 3 carcinoids, which are larger and more aggressive, may exhibit ulceration and are often associated with distant metastases [3].
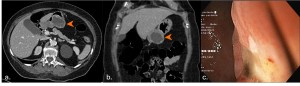
Metastases
Metastatic involvement of the stomach is rare but can occur via hematogenous spread (melanoma, breast, lung and ovarian cancers), direct extension (pancreatic cancer), or lymphatic spread (esophageal cancer). CT findings include submucosal nodules, diffuse wall thickening, or a limits plastica appearance [6].
In patients with a known primary malignancy, the presence of submucosal lesions on CT, especially in cancers prone to gastric metastasis, should prompt consideration of gastric metastasis. Endoscopic biopsy is recommended for confirmation in such cases [5].
Benign Gastric Tumors
Gastric Lipoma
Lipomas are benign submucosal masses that are well-defined and homogeneous, with fat attenuation (-70 to -120 HU). They are usually asymptomatic but can lead to outlet obstruction or intussusception if they are large and located near the gastric pylorus [5].
Gastric Leiomyoma
Leiomyomas are typically submucosal tumors that present as smooth, well-defined masses with homogeneous low enhancement and endoluminal growth pattern. They are usually less than 5 cm in size, although large tumors may ulcerate or perforate. [8].
Inflammatory Conditions
Gastritis
Gastritis is a common stomach condition characterized by inflammation in the stomach wall. CT scans may show either diffuse or focal thickening of the wall, typically with increased enhancement of the mucosa and a hypodense submucosal layer due to edema, often presenting a "halo" appearance [5].
Peptic Ulcers
Peptic ulcers, often caused by H. pylori or NSAIDs, may show mucosal disruption, luminal outpouching, wall thickening, or hyperenhancement on CT. Complications like perforation (extraluminal gas) or bleeding (contrast extravasation) are detectable. Focal, eccentric wall thickening >1 cm suggests malignancy, warranting endoscopy. CT aids in diagnosing and localizing bleeding sources [5, 8].
Other Conditions
Gastric Pneumatosis
Gastric pneumatosis can be seen on CT as linear or cystic gas collections within the gastric wall. Gas in the rugae can mimic pneumatosis, so sagittal/coronal reconstructions can help with the diagnosis. Emphysematous gastritis, a life-threatening condition, is characterized by mottled air in the gastric wall with associated thickening [8].
Bezoars
Bezoars are intraluminal masses formed from ingested materials like hair (trichobezoars), vegetable matter (phytobezoars), milk (lactobezoars), or medications (pharmacobezoars). They appear on CT as mobile gastric filling defects with a mottled appearance due to trapped air. While often confined to the stomach, they can extend into the intestines (Rapunzel syndrome) [3].
Gastric Volvulus
Acute gastric volvulus is a surgical emergency due to risks of ischemia, perforation, and necrosis. Types include organoaxial (most common), mesenteroaxial, and mixed. MDCT shows antrum displacement above the fundus and antropyloric transition point. Organoaxial involves stomach rotation along the long axis, while mesenteroaxial rotates along the short axis [9].
Ectopic Pancreas
Ectopic pancreas presents as an ill-defined submucosal mass with endoluminal growth, usually in the distal antrum. It has enhancement similar to pancreatic tissue and may exhibit a central ductal structure on high-resolution CT. [3].
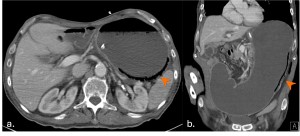
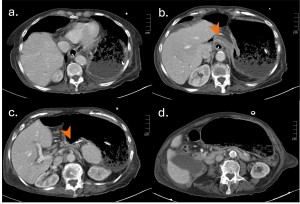
Gastric Varices
Gastric varices arise from flow reversal in the gastric fundal venous plexus, often due to portal hypertension from cirrhosis or splenic vein thrombosis. CT shows dilated, contrast-filled vessels along the lesser curvature, often contiguous with esophageal varices. Bleeding is less frequent but more severe than esophageal varices, with higher mortality. CT also visualizes afferent/efferent veins and collateral vessels [8].
Gastric Diverticulum
Gastric diverticula are sac-like outpouchings that typically arise from the posterior surface of the gastric fundus near the spleen, adrenal gland, and left diaphragm. On CT scans, they appear as thin-walled cystic lesions with an air-fluid level [10].