Crohn’s disease manifests variably, depending on the area involved.
Common symptoms included:
- abdominal pain (usually in the right lower quadrant),
- diarrhea,
- weight loss,
- fatigue,
- fever,
- nausea,
- vomiting.
Severe cases presented with:
- intestinal obstruction and even intestinal perforation,
- rectal bleeding,
- perianal disease (fissures, abscesses, fistulas).
The main imagining modalities used were:
- plain abdominal radiographs (mainly used for detecting bowel obstruction and perforation)
- ultrasound (useful for evaluating bowel wall thickening, hyperemia, and abscesses)
- computed tomography (the gold standard for emergency evaluation)
- magnetic resonance imaging (provides superior soft–tissue contrast).
The radiological findings were:
- bowel mural thickening (most frequently observed in the terminal ileum)
- „skip lesions” - interspersed inflammation ''skipping'' parts of the bowel left unaffected
- different patterns of wall enhancement (the mesenteric border is more often affected); it can be stratified (bilaminar or trilaminar) – „target sign” or homogeneous (transmural hyperenhancement).
- densification of mesenteric fat
- engorged vasa recta
- lymphadenopathy
- bowel strictures with or without intestinal occlusion
- fistulas – communication between two epithelial lined organs (internal fistula) – entero-enteral, entero-sigmoid, entero-vesical, etc., or communication with the skin surface (external fistula);
- abscesses: fluid collection with rim wall enhancement
- bowel perforation
The treatment of Crohn’s Disease focuses on controlling inflammation, inducing and maintaining remission, and preventing complications. Corticosteroids have a rapid onset of action and were indicated to induce remission in Crohn's Disease. Immunosuppressants and biologic agents were used for maintenance therapy. In severe cases, surgical resection of the inflamed bowel was performed. Surgery was also performed for complications such as strictures, bowel perforation, or fistulas.
In the following, we will present a few characteristic cases that were admitted to our hospital and their imaging findings:
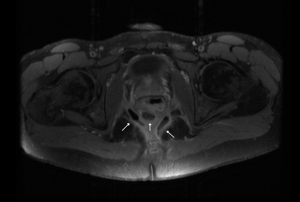
CASE 1.
A 23-year-old male patient underwent his first MRI during the initial hospitalization, which confirmed the diagnosis of Crohn’s Disease.
The imaging revealed:
- multiple transsphincteric and extrasphincteric fistulas
- multiple collections involving the levator ani muscle
- incomplete fistulous tracts in the ischiorectal fossa.
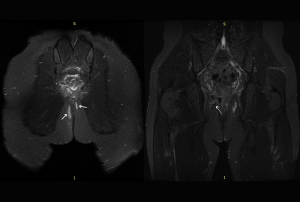
The MRI reevaluation two months after the initial diagnosis and following conservative (non-biologic) treatment revealed the previously described fistulas, which now exhibit complete fistulous tracts with a visible external opening. The previously noted collections appear more organized at this stage.
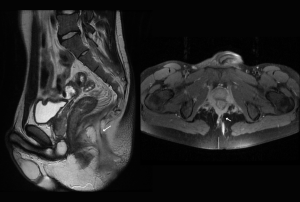
Surgical intervention was performed to excise the previously identified fistulas. Six months postoperatively, imaging revealed a newly developed intersphincteric fistulous tract with a visible external opening.
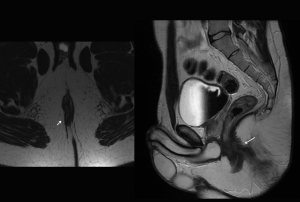
Two years later, the patient presented to the hospital for imaging reevaluation. The MRI revealed a complex fistulous tract forming a horseshoe perianal abscess.
This case highlights the chronic and relapsing nature of perianal Crohn’s Disease, characterized by the formation of recurrent and complex fistulas, despite initial treatment and surgical intervention. Although the patient underwent surgical excision and conservative management, disease progression led to the development of a horseshoe-shaped perianal abscess, emphasizing the challenging nature of fistulizing Crohn’s Disease.
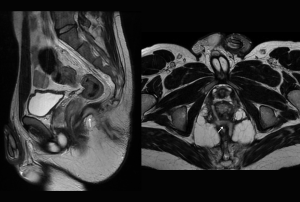
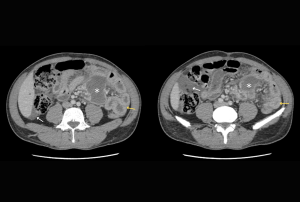
CASE 2.
A 32-year-old patient with a history of appendectomy was admitted to our clinic and diagnosed with Crohn’s Disease based on the investigations performed during hospitalization.
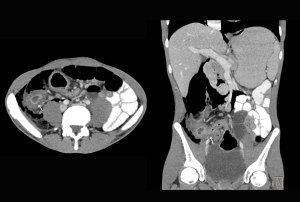
CT findings at admission revealed:
- significant inflammatory changes in the cecum and terminal ileum, with diffuse intestinal wall thickening measuring 11–12 mm.
- marked inflammatory changes in the mesentery, with a poorly defined, irregular intramesenteric abscess surrounded by multiple areas of mesenteric fat stranding.
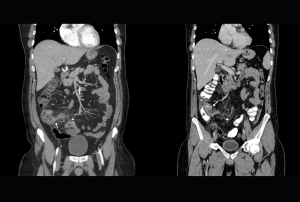
This case illustrates a complicated presentation of Crohn’s Disease, confirmed shortly after the patient’s admission. Prompt diagnosis and management are critical in such cases to prevent further complications like bowel perforation or fistula formation.
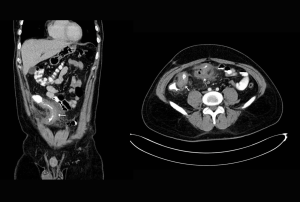
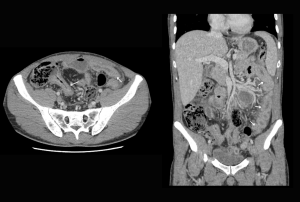
CASE 3.
A 37-year-old female patient, previously diagnosed with Crohn’s Disease and currently not receiving maintenance therapy, was admitted for severe abdominal pain.
CT findings at admission revealed:
- circumferential wall thickening with associated mucosal enhancement in the cecum and ascending colon, extending to the terminal ileum, with a stenotic appearance and upstream bowel dilation, accompanied by air-fluid levels.
- a well-organized, multilobulated collection with iodophilic walls located in the right iliac fossa, showing a tendency to cutaneous fistulization.
This case demonstrates a complicated form of Crohn’s Disease. The circumferential wall thickening and stenosis suggest advanced inflammatory and fibrotic changes, leading to partial bowel obstruction. Additionally, the multilobulated collection in the right iliac fossa with a tendency for cutaneous fistulization indicates a progression to fistulizing disease, a challenging complication.
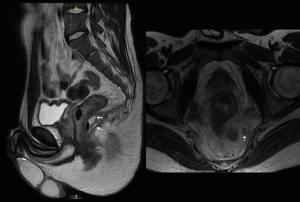
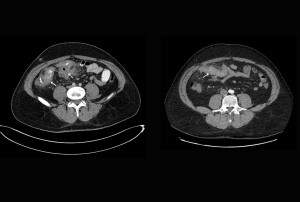
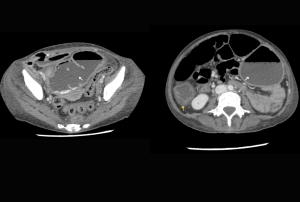
CASE 4.
A 42-year-old male with a history of Crohn’s Disease on maintenance therapy presented with a deterioration in general condition and diffuse abdominal pain.
CT findings revealed:
- diffuse bowel wall thickening involving non-dilated intestinal loops, including the terminal ileum, consistent with active inflammatory changes.
- intramesenteric abscess along with additional organized collections.
- pelvic ileal loops adherent to each other and to the superior wall of the urinary bladder, which appeared thickened with mucosal edema and small air accumulations, indicating the presence of a vesicoenteric fistula.
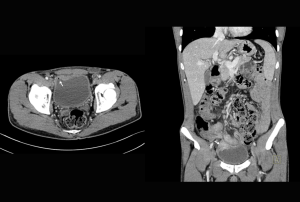
This case represents a severe and complex form of Crohn’s Disease, with findings indicating active inflammation, intra-abdominal abscesses, and a vesicoenteric fistula, a serious complication.
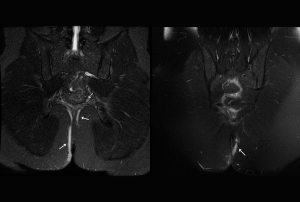
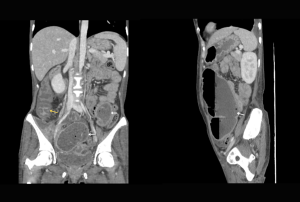
CASE 5.
A 25-year-old male with a known history of Crohn’s Disease presented to the emergency department with diffuse abdominal pain.
CT findings at admission revealed:
- large-volume pneumoretroperitoneum and pneumoperitoneum, predominantly in the right abdominopelvic region.
- the terminal ileum showed diffuse inflammatory wall thickening with a narrowed lumen, causing moderate upstream intestinal distension.
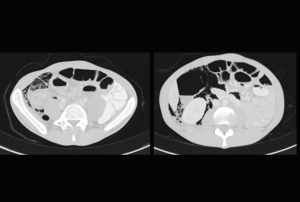
Given the clinical deterioration and imaging findings, an emergency surgical intervention was performed.
During surgery, an extensive fecal collection was identified in the right iliac fossa, confirming intestinal perforation. The perforation measured approximately 2 cm in diameter and was located in an intestinal segment with significant wall thickening and severe inflammatory changes, making anatomical identification challenging. Multiple adhesions were noted between adjacent bowel loops and surrounding structures.
A limited segmental bowel resection of the affected segment was performed
The patient recovered without complications and was discharged in stable condition.
The presented cases illustrate the variable and complex nature of Crohn’s Disease, ranging from intestinal wall thickening and abscesses to severe complications such as vesicoenteric fistulas and intestinal perforation. Despite initial treatment, the chronic relapsing course of Crohn’s Disease can lead to recurrent complications, emphasizing the need for multidisciplinary care and long-term monitoring.
These cases demonstrate the significance of integrating radiology into clinical decision-making for successfully managing Crohn’s Disease and preventing potentially life-threatening complications.