The aim of treatment options in Pelvic Congestion Syndrome (PCS) is to resolve venous congestion and thereby alleviate the associated symptoms. Percutaneous endovascular embolization of the pelvic venous plexuses represents the most commonly utilized interventional treatment for PCS. Although most of the literature focuses on female patients, we have applied the same therapeutic procedure in men, given that the underlying pathophysiological mechanism is conceptually similar (Dabbs et al., 2018).
The procedure can be divided into three main steps:
- Vascular Access: Vascular access is obtained under ultrasound guidance, either via the right common femoral vein or the right internal jugular vein. Although access through the basilic or cephalic veins is possible, these routes have not proven to be more advantageous for catheterizing the pelvic venous plexuses (Kashef et al., 2023).
- Venography: After catheterization of the left internal iliac vein using a 5Fr catheter (Cobra 2 or Simmons 1 if access is via the inferior vena cava; MPA 2 if access is via the superior vena cava), venography of the pelvic venous plexuses is performed. It is essential to carry out the venography both at rest and during a Valsalva maneuver to identify any contrast reflux. (Kashef et al., 2023; Koo & Fan, 2014)
 Fig 1: A 65-year-old male presented with chronic pelvic pain persisting for 3 years, exacerbated by prolonged standing and sexual intercourse. Left internal iliac vein venogram shows varicose ectasia of the paravesical, paraprostatic and pudendal plexus (arrow).
Fig 1: A 65-year-old male presented with chronic pelvic pain persisting for 3 years, exacerbated by prolonged standing and sexual intercourse. Left internal iliac vein venogram shows varicose ectasia of the paravesical, paraprostatic and pudendal plexus (arrow). - Embolization: Embolization is typically carried out using various agents such as sclerosants, coils, plugs, or combinations thereof.
- Sclerosant Agents: When sclerosants are used, temporary target occlusion is achieved with a balloon catheter (stop-flow technique) to prevent the dispersion of the embolic agent and to increase its downstream concentration. Subsequently, the sclerosant (usually a mixture of 3% sodium tetradecyl sulfate with an equal volume of 5% iodinated sodium morrhuate combined with gelfoam) is injected under fluoroscopic guidance and allowed to act for 5-10 minutes. (Koo & Fan, 2014)
 Fig 2: Stop-flow technique: temporary target occlusion is achieved with a balloon catheter (arrow) to prevent the dispersion of the embolic agent and to increase its downstream concentration
Fig 2: Stop-flow technique: temporary target occlusion is achieved with a balloon catheter (arrow) to prevent the dispersion of the embolic agent and to increase its downstream concentration - Coils and Plugs: The coils selected should have a diameter approximately 20% greater than that of the target vessel. Distal embolization is performed using pushable coils, while detachable coils are preferred proximally to reduce the risk of distal migration. Embolization with coils below the inguinal ligament is not recommended, as it may be palpable and cause long-term discomfort for the patient (Kashef et al., 2023)Occlusive detachable plugs are used only in select cases due to their higher cost and the lack of evidence in the literature demonstrating superior efficacy compared to coils. (Guirola et al., 2018)
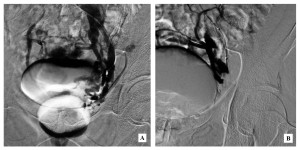
 Fig 3: A 31-year-old male with a history of left varicocele, previously treated with ligation of the spermatic vein seven years earlier, presented with pelvic pain. Diagnostic phlebography revealed ectasia of collateral vessels originating from the left internal spermatic vein and communicating with the lumbar vein plexus, contralateral side, and pelvic region (A). Placement of a 12×9 mm plug (arrow) for occlusion of the left internal spermatic vein.(B)
Fig 3: A 31-year-old male with a history of left varicocele, previously treated with ligation of the spermatic vein seven years earlier, presented with pelvic pain. Diagnostic phlebography revealed ectasia of collateral vessels originating from the left internal spermatic vein and communicating with the lumbar vein plexus, contralateral side, and pelvic region (A). Placement of a 12×9 mm plug (arrow) for occlusion of the left internal spermatic vein.(B)
In cases where PCS is associated with May-Thurner syndrome, treatment involves the placement of a stent in the common iliac vein. This may be combined with embolization of the pelvic varicosities to further improve the success rate in alleviating symptoms. (Gavrilov et al., 2020)
After embolization, repeat venography is performed to confirm successful occlusion and to ensure that no residual venous reflux persists. Early follow-up indicates a notable improvement in pelvic pain and related symptoms.