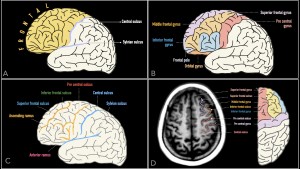
FRONTAL LOBE: bounded anteriorly by the frontal pole and posteriorly by the central sulcus which separates it from the parietal lobe.
The superior and inferior frontal sulci divide the anterior portion of the frontal lobe into:
- Superior frontal gyrus
- Middle frontal gyrus
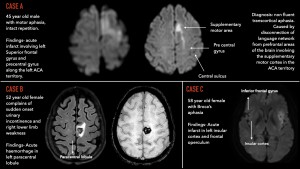
- Inferior frontal gyrus (includes Broca’s area)
- Damage to Broca’s area causes motor/expressive aphasia.
Precentral Gyrus
- The precentral gyrus runs anterior and parallel to the central sulcus and is bounded anteriorly by the precentral sulcus
- It houses the primary motor cortex, which represents the motor map (homunculus).
- Lesion results in contralateral hemiparesis.
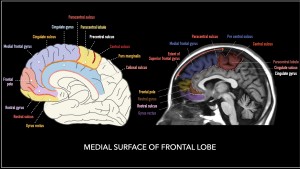
Medial Surface of the Frontal Lobe
- The superior frontal gyrus continues onto the medial surface and is divided into two parts by the paracentral sulcus:
- Medial frontal gyrus (anteriorly)
- Paracentral lobule (posteriorly upto precentral sulcus)
- The supplementary motor area (SMA) lies in the medial frontal gyrus, anterior to the paracentral lobule.
- The cingulate gyrus is located above the callosal sulcus and parallels the corpus callsoum. The cingulate sulcus, located above the cingulate gyrus, continues as pars marginalis posterio-superiorly.
Paracentral Lobule
- The paracentral lobule is mainly the medial continuation of the precentral gyrus (frontal lobe) and the postcentral gyrus (parietal lobe).
- It is bounded by the paracentral sulcus (anteriorly) and the pars marginalis (posteriorly).
- The anterior two-thirds of the paracentral lobule are part of the primary motor cortex, representing the foot and regulating cortical inhibition of bladder and bowel voiding.
Inferior (Olfactory) Surface: The rostral sulcus divides it into:
- Rostral gyrus (superiorly)
- Gyrus rectus (inferiorly)
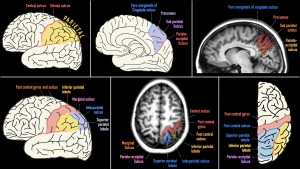
PARIETAL LOBE:
Boundaries
- Anterior: Central sulcus.
- Posterior: Parieto-occipital sulcus.
Postcentral Gyrus
- Located immediately anterior to the postcentral sulcus.
- Contains the primary somatosensory cortex, responsible for processing sensory input from the contralateral side of the body.
- Lesion: Results in contralateral sensory deficits
Interparietal Sulcus divides the lateral surface into:
- Superior parietal lobule
- Inferior parietal lobule
Inferior Parietal Lobule
- Supramarginal gyrus: Caps the Sylvian sulcus.
- Angular gyrus: Caps the superior temporal sulcus.
- Functions: Involved in sensory integration, language processing, and spatial awareness.
Medial Surface
- Precuneus: Extends from the pars marginalis (anteriorly) to the parieto-occipital sulcus (posteriorly).
- Paracentral lobule posterior to central sulcus: Medial continuation of the postcentral gyrus. Considered part of the parietal lobe.
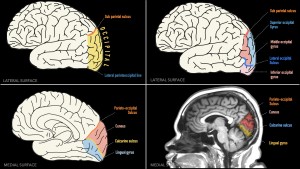
OCCIPITAL LOBE: bordered medially by parieto-occipital sulcus and laterally by the Lateral parietotemporal sulcus.
Medial surface: from superior to inferior-
- Parieto-occipital sulcus
- Cuneus
- Calcarine sulcus (primary visual cortex)
- Lingual gyrus.
Lateral surface is highly variable, consisting of superior, middle and inferior occipital gyrus.
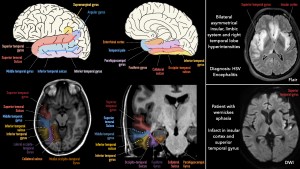
TEMPORAL LOBE:
- Superior Border: Sylvian sulcus.
- Inferolateral Border: Lateral parietotemporal sulcus (imaginary line from the pre-occipital notch to the parieto-occipital sulcus).
Divisions
- Neocortex: Lateral and inferolateral regions.
- Medial Temporal Lobe (Limbic Lobe):
- Hippocampus: memory consolidation.
- Amygdala: emotional regulation and memory.
- Parahippocampal gyrus (PHG): Spatial and contextual memory.
Lateral Surface: Divided by the superior temporal sulcus and inferior temporal sulcus into:
- Superior temporal gyrus (STG): Posterior portion houses Wernicke’s area (responsible for language comprehension), bordered by the angular gyrus.
- Middle temporal gyrus (MTG): Involved in semantic memory and visual association.
- Inferior temporal gyrus (ITG): Plays a role in object recognition and visual processing.
Inferior Surface (from medial to lateral)
- Parahippocampal gyrus:
- Anteriorly: curves to form the uncus of the temporal lobe.
- Posteriorly: continuous with the lingual gyrus.
- Collateral sulcus
- Fusiform gyrus (lateral occipitotemporal gyrus)
- Occipitotemporal sulcus
- Inferior temporal gyrus
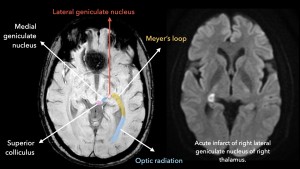
HIPPOCAMPUS: Divided into three parts based on midbrain landmarks:
1. Head of the Hippocampus
- Extends from the basilar artery to the interpeduncular cistern.
- Features hippocampal digitations, collectively known as the pes hippocampus.
2. Body of the Hippocampus
- Extends from the interpeduncular cistern to the superior colliculus.
- Composed of two interlocking gyri:
- Cornu Ammonis (CA)
- Dentate Gyrus
- The unique arrangement gives it a Swiss roll appearance.
- Cornu Ammonis is subdivided into four regions (CA1 to CA4).
- The alveus, a layer of white matter on the superior surface, continues medially to form the fimbria.
- Subiculum, located superior to the parahippocampal gyrus, serves as a bridge connecting the Cornu Ammonis to the parahippocampal gyrus.
3. Tail of the Hippocampus
- Located posterior to the superior colliculus
- Continues into the subsplenial gyrus.

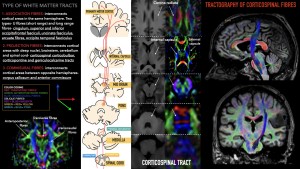
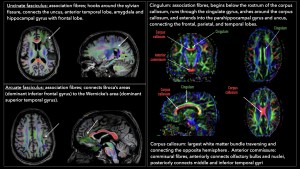
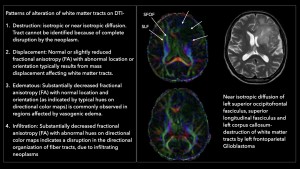
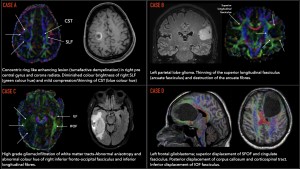
DIFFUSION TENSOR IMAGING (DTI):
Anatomy of white matter tracts on DTI and various patterns of alteration caused by neoplasms.

MIDBRAIN
The midbrain has two primary regions: the ventral tegmentum and the dorsal tectum (quadrigeminal plate). The tegmentum houses brainstem nuclei, while the tectum includes the quadrigeminal plate with the superior and inferior colliculi. The cerebral aqueduct connects the third and fourth ventricles and is surrounded by periaqueductal gray matter.
Case A: Internuclear Ophthalmoplegia (INO)
INO results from a lesion in the medial longitudinal fasciculus (MLF), causing impaired adduction of the ipsilateral eye and horizontal nystagmus in the contralateral abducting eye.
Case B: Parinaud Syndrome
Also known as dorsal midbrain syndrome, this condition arises from a lesion in the superior tectal plate and presents with a triad:
- Upward gaze palsy (often with diplopia)
- Light-near dissociation (pupils react to near stimuli but not light)
- Convergence-retraction nystagmus (jerky eye movements during upward gaze attempts).
Case C: Progressive Supranuclear Palsy (PSP)
PSP, a neurodegenerative tauopathy, manifests with vertical gaze palsy, postural instability, falls, Parkinsonian features, and cognitive decline. Imaging shows midbrain atrophy, with a sagittal “hummingbird sign” due to loss of brainstem convexity. Mickey mouse sign: reduction in the anteroposterior diameter in the midline (from interpeduncular fossa to the intercollicular groove).

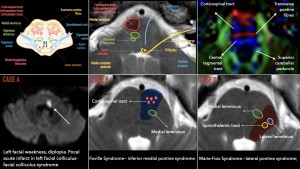
PONS: bulbous structure divided into two main regions:
- Basis Pontis (Ventral Part):
- Contains white matter tracts, including the corticospinal, corticobulbar, and corticopontine tracts.
- Transverse fibers dominate its bulk.
- Pontine Tegmentum (Dorsal Part):
- Continuous with the tegmentum of the medulla and midbrain.
- Houses white matter tracts like the medial and lateral lemnisci.
- Contains cranial nerve nuclei for trigeminal (V), abducens (VI), facial (VII), and vestibulocochlear (VIII) nerves.
CASE A: Facial Colliculus Syndrome
- Lesion at the facial colliculus on the floor of the fourth ventricle.
- Structures Affected: Facial nerve genu fibers, abducens nerve, and medial longitudinal fasciculus (MLF).
- Lower motor neuron facial palsy (loss of taste in the anterior two-thirds of the tongue, hyperacusis).
- Horizontal conjugate gaze palsy.
- Diplopia.
CASE B: Foville Syndrome (Inferior Medial Pontine Syndrome)
- Infarct involving the corticospinal tract, medial lemniscus, MLF, paramedian reticular formation, and abducens and facial nerve nuclei.
- Contralateral hemiparesis
- Ipsilateral facial nerve palsy.
- Hemi-sensory loss.
- Gaze palsy with an inability to gaze toward the lesion side and diplopia.
CASE C: Marie-Foix Syndrome (Lateral Pontine Syndrome)
- Cause: Infarction of the lateral pons and middle cerebellar peduncle involving the corticospinal, spinothalamic, and cerebellar tracts and the facial and vestibulocochlear cranial nerve nuclei.
MEDULLA
- Ventral (Anterior) Medulla:
-
- Olive: Contains inferior olivary nucleus, associated with motor coordination.
- Pyramids: Carry corticospinal tracts.
- Rootlets of cranial nerves IX–XII (Glossopharyngeal, Vagus, Accessory, and Hypoglossal nerves).
- Tegmentum (Dorsal) Medulla:
-
- Cranial nerve nuclei
- White matter tracts
Hypertrophic Olivary Degeneration (HOD)
- Neurological condition with distinct pattern of transsynaptic degeneration characterized by hypertrophy of the inferior olivary nucleus.
- Typically results from lesions in the brainstem or cerebellum disrupting the triangle of Guillain and Mollaret (dentatorubro-olivary pathway)- A neural loop connecting three structures:
-
- Red nucleus (midbrain).
- Inferior olivary nucleus (medulla).
- Contralateral dentate nucleus (cerebellum).
Area postrema syndrome:
Affects the chemoreceptor trigger zone on the medial posteroinferior medulla, presenting with persistent hiccups, nausea, and/or vomiting lasting over 48 hours.
Dejerine syndrome: affects the hypoglossal nerve nucleus from occlusion of small perforating branches.

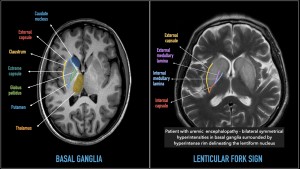
BASAL GANGLIA
Anatomically : 3 paired nuclei called the corpus striatum-
- Caudate nucleus
- Lentiform nucleus
- Putamen
- Globus pallidus
Additional functional nuclei include:
- Subthalamic nuclei
- Substantia Nigra
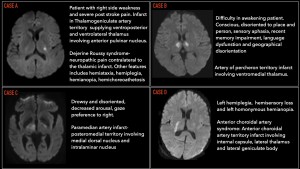
THALAMUS:
Demonstrating various patterns of thalamic infarcts helps correlate specific nuclei involvement with associated clinical syndromes.
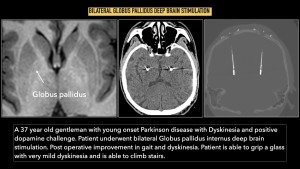
DEEP BRAIN STIMULATION (DBS)
The subthalamic nucleus (STN) is a densely packed, lens-shaped structure composed mainly of glutamatergic projection neurons. DBS electrodes are placed near the dorsal subthalamic nucleus in Parkinson disease. Motor symptoms like bradykinesia and rigidity are linked to exaggerated beta (15–30 Hz) oscillations in STN local field potentials, which are reduced by high-frequency DBS, improving motor function.
The STN (indirect pathway) and GPi (direct pathway) both improve PD motor symptoms when their sensorimotor regions are stimulated. The GPi is larger (~450 mm³) than the STN (~150 mm³), with GPi DBS primarily providing antidyskinetic effects.