Congress:
ECR25
Poster Number:
C-11922
Type:
Poster: EPOS Radiologist (educational)
DOI:
10.26044/ecr2025/C-11922
Authorblock:
C. H. Hernández García, C. Buendía Pajares, A. Martín González, I. Solis Muñiz, S. I. Sirvent Cerdá; Madrid/ES
Disclosures:
Carmen Hernández Hernández García:
Nothing to disclose
Claudia Buendía Pajares:
Nothing to disclose
Alba Martín González:
Nothing to disclose
Inés Solis Muñiz:
Nothing to disclose
Sara Inmaculada Sirvent Cerdá:
Nothing to disclose
Keywords:
Paediatric, MR, Education, Developmental disease
- Study protocol:
- Normal study:
- T1 without gadolinium:
- Adenohypophysis and stalk: similar to cortex (except in neonates and pregnant women which is hyperintense).
- Neurohypophysis:
- Hyperintense (neurosecretory granules composed of neurophysin transporter protein and anti-diuretic hormone).
- Isointense (10-15%): suspected traumatic or post-surgical damage.
- Absent: central diabetes insipidus.
- T1 with gadolinium: Early, intense and homogeneous enhancement of the infundibulum and neurohypophysis, followed by an intense, progressive and sequential uptake of the adenohypophysis from its junction with the stalk towards the periphery (the onset of infundibular enhancement and vascular tuft should be synchronous with the appearance of contrast in the internal cerebral veins).
- T2: Adenohypophysis and stalk similar to the cortex.
 Fig 1: Figure 1: 7yo boy with normal pituitary gland.
Fig 1: Figure 1: 7yo boy with normal pituitary gland.
- T1 without gadolinium:
- Differences exists in pituitary size depending on age:
- HlPOPITUITARY DEVELOPMENTAL ANOMALIES
- Agenesis or hypoplasia: Sella turcica scarcely excavated with pituitary volume <3mm, concave morphology and adapted to the sellar floor (hypoplasia).
- They usually present multiple, permanent hormonal deficits and are more frequently associated with other congenital anomalies or systemic or CNS syndromes.
- Ectopic neurohypophysis: the neurohypophysis is not identified in its usual location.
- High predictive value for the diagnosis and prognosis of GH deficiency: the higher the location, the greater the GH deficiency and the better the response to treatment.
- The pituitary stalk can be normal, hypoplastic or absent.
- For correct evaluation: dynamic sequence in sagittal plane after gadolinium.
- Pituitary stalk transection syndrome: small adenohypophysis, interrupted pituitary stalk and ectopic neurohypophysis: pituitary dwarfism.
 Fig 3: Figure 3: Male 4yo with short stature: T1 hypersignal focus of the neurohypophysis in ectopic location in the infundibulum (red arrow). Minimal calibre pituitary stalk only visible after gadolinium administration, well centred in the midline. Adenohypophysis of small size (hypoplasia), normal signal intensity.
Fig 3: Figure 3: Male 4yo with short stature: T1 hypersignal focus of the neurohypophysis in ectopic location in the infundibulum (red arrow). Minimal calibre pituitary stalk only visible after gadolinium administration, well centred in the midline. Adenohypophysis of small size (hypoplasia), normal signal intensity.
- Duplicación pituitary.
- Septo-optic dysplasia: Within the spectrum of holoprosencephaly (midline defects) - Brain insult that alters diencephalon-derived structures.
- Hypoplasia or agenesis of the optic pathway (fascicles, chiasm and optic ribbons).
- Partial or complete agenesis of the septum pellucidum and/or cortical malformations.
- Dysfunction of the EHH (30%).
- Clinical expression is variable: impaired vision, growth retardation due to GH and TSH deficiency, autism, obesity...
- Agenesis or hypoplasia: Sella turcica scarcely excavated with pituitary volume <3mm, concave morphology and adapted to the sellar floor (hypoplasia).
-
- Kallman’s syndrome: Genetic syndrome (+ sporadic fc).
- Hypogonadotropic hypogonadism (GnRH deficiency) + anosmia/hyposmia.
- Failure of olfactory cell migration from the olfactory placode to the hypothalamus.
- Absence or hypoplasia of olfactory bulbs is demonstrable on coronal/sagittal T2.
- Pituitary and hypothalamus are usually normal.
- Kallman’s syndrome: Genetic syndrome (+ sporadic fc).
-
- Hypothalamic hamartoma: benign non-neoplastic heterotopias typically occurring in the region of the hypothalamus and arising from the tuber cinereum (between the mammillary bodies and the optic chiasm).
- Clinical: gelastic seizures, visual problems, precocious puberty and behavioural problems.
- Types: sessile (attached to mammillary bodies) or pedunculated (projecting into suprasellar cistern).
- Characteristics: T1: Hypointense to cerebral cortex (74%); T1 + Gd: No contrast enhancement; T2: Hyperintense to cerebral cortex (93%), more noticeable in FLAIR (the higher the proportion of glial cells, the higher the T2 signal).
- Medical treatment of precocious puberty and qx only if intractable epilepsy.
- Hypothalamic hamartoma: benign non-neoplastic heterotopias typically occurring in the region of the hypothalamus and arising from the tuber cinereum (between the mammillary bodies and the optic chiasm).
-
- Persistent craniopharyngeal groove: Communication through the base of the skull between the nasopharynx and the pituitary fossa.
- Type 1: thin (incidental).
- Type 2: with ectopic adenohypophysis.
- Type 3A: with cephalocele.
- Type 3B: with tumour.
- Type 3C: with both.
- Clinical: asymptomatic, liquorrhoea, intracranial hypotension, pituitary prolapse (mass in nasopharynx), association with craniofacial anomalies.
- Persistent craniopharyngeal groove: Communication through the base of the skull between the nasopharynx and the pituitary fossa.
-
- Rathke's cyst: Non-neoplastic lesions originating from embryological remnants of Rathke's pouch (or pituitary diverticulum).
- Selar or suprasellar.
- They increase in size due to fluid secretion (congenital but + seen in adults).
- Well-demarcated lesions, homogeneous signal: in T1 and T2 very variable (typically inapparent in some of the two sequences), without enhancement; Hyper T1 due to protein content (50%).
- Clinical: visual disturbances, headache, pituitary disturbances.
- Resection if clinical.
- Intracystic nodule (60-75%): Hyperintense in T1 and hypointense in T2.
- Rathke's cyst: Non-neoplastic lesions originating from embryological remnants of Rathke's pouch (or pituitary diverticulum).
-
- Cephalocele: herniation of brain tissue through a cranial defect. They can occur in different locations, the sphenoid being extremely rare.
- Lipoma: the result of an abnormal differentiation of the embryological primitive meninx, and therefore can have different locations (suprasellar 15%) and can be associated with other anomalies. They are usually asymptomatic and incidental findings at any age.
- Hyperintense on T1 and T2, which is suppressed with fat suppression techniques, without enhancement after Gd. Often crossed by cranial nerves and vessels.
-
- Epidermoid cyst: Inclusion of ectodermal elements with presence of appendages such as hair and sebaceous cysts.
- Isosintense to CSF on T1 and T2 although variable.
- T1 + IVC sometimes peripheral enhancement.
- Hyper in DWI.
- Epidermoid cyst: Inclusion of ectodermal elements with presence of appendages such as hair and sebaceous cysts.
-
- Dermoid cyst: Developmental abnormality of the ectoderm.
- T1 hyperintense (cholesterol).
- T1 C+ (Gd): no enhancement. Pial enhancement if rupture.
- T2: variable signal ranging from hypo to hyperintense.
- Dermoid cyst: Developmental abnormality of the ectoderm.
-
- Arachnoid cyst: 1% intracranial lesions.
- Benign CSF-filled lesions with thin walls and no solid part.
- Asymptomatic.
- Obstructive hydrocephalus.
- Arachnoid cyst: 1% intracranial lesions.
- Whole skull: Sag T1 SE, Ax and Cor T2 TSE, Ax FLAIR, DWI (B0, B1000 and ADC), SWI.
- Selar region: Sag and Cor T1 TSE, Sag T2 TSE, Sag and Cor T1, Dynamic 3DT1 postgadolinium.
- Children (<12 years): 3-6mm (flat or slightly concave upper surface).
- Puberty: convex upper surface; 10-12mm female and 7-8mm male.
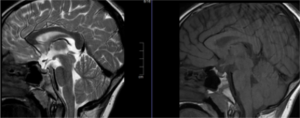
Fig 2: Figure 2: Normal pubertal bulging pituitary gland in 13-year-old girl.
- Adult: Young: Male: 8mm / Female: 9mm // Pregnancy: 12mm // Older (>50 years): gradually decreases in size (<3mm pathological).
**If larger for age, administer IVC to rule out intraglandular lesion.
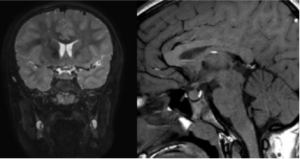
Fig 4: Figure 4: Child 11yo with strabismus and volume loss of the left optic nerve: Volume loss with hypoplasia of the left optic nerve and left chiasm (arrow). No evidence of neurohypophysis in normal or ectopic location, absence of septum pellucidum (circle).
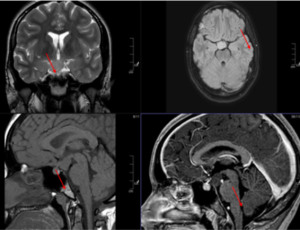
Fig 5: Figure 5: Girl 7yo with gelastic crisis. Pseudonodular lesion dependent on the tuber cinereum. Hypo/isointense to the cerebral cortex in T1, without enhancement after gadolinium. Hyperintense cerebral cortex on T2, more noticeable on FLAIR. Findings compatible with hypothalamic hamartoma.
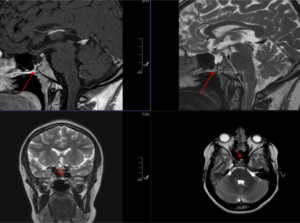
Fig 6: Figure 6: Elongated sella turcica with hypophyseal descent + 2 mm patent type II craniopharyngeal canal (red arrow).
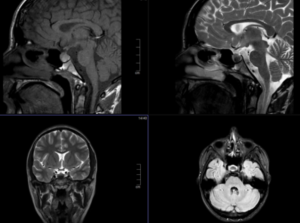
Fig 7: Figure 7: Female 16yo. 7 mm rounded lesion, hyperintense in T1 and hypointense in T2 in the posteroinferior margin of the adenohypophysis compatible with Rathke's pouch cyst.

Fig 8: Figure 8: Child 6yo with autism spectrum disorder. Incidental focal lesion in relation to the pituitary stalk and extending to the hypothalamic region, hyperintense in T1, which is suppressed with fat suppression techniques, measuring 8x5mm, without reaching the sellar diaphragm, compatible with lipoma of the pituitary stalk.
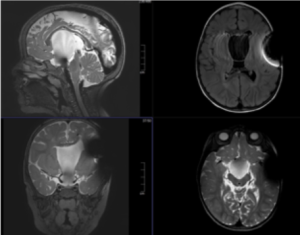
Fig 9: Figure 9: Epidermoid cyst.
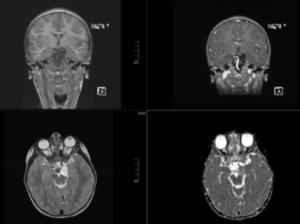
Fig 10: Figure 10: Dermoid cyst.
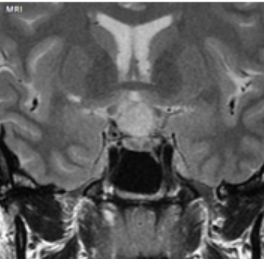
Fig 11: Figure 11: Arachnoid cyst.