The site of involvement influences differences in tumor staging and nodal compromises, especially in the early stages.
Clinical Staging: (Table 2)
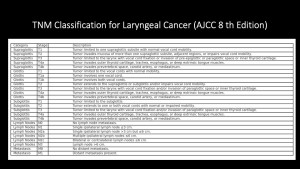
Tumor staging is the most relevant prognostic factor and is essential to decide the appropriate treatment:
- early stages (0-II) usually undergo radiation therapy or surgery only.
- advanced stages (III-IV) are generally treated with a combination of radiation therapy (with concurrent chemotherapy) and surgery (typically including selective or radical neck dissection)
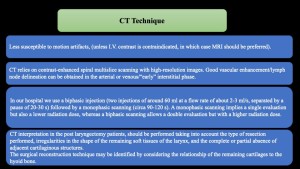
CT Technique: See Table 3
Surgical Treatment Options
- Partial (conservative) laryngectomy, especially for early (T1-T2) supraglottic/glottic tumors.
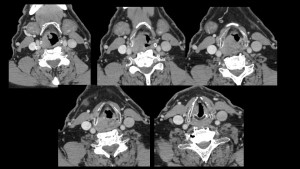
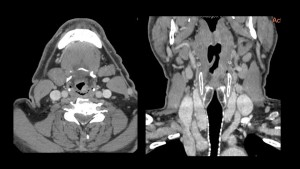
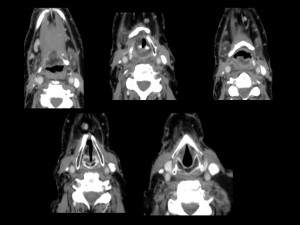
- Radiation therapy result in similar rates of survival and local control; however, for superior results with regard to voice preservation, patients with early-stage glottic carcinomas usually undergo radiation therapy instead of surgery. See (Fig 5): well-differentiated squamous cell carcinoma in right transglottic T1b2N0M0 subglottic involvement and (Fig 6) Post radical radiotherapy.
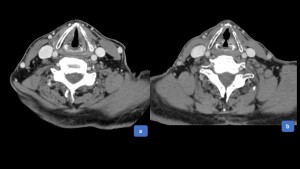
 Fig 5: Axial CT scan in a 82 year-old man shows asymmetry of the right vocal cord with thickening due to an irregular lesion, in the middle and anterior third of the vocal cord that infiltrates the anterior commissure and anterior third of the left vocal cord and right subglottis Dx: well-differentiated squamous cell carcinoma in right transglottic T1b2 subglottic involvement
Fig 5: Axial CT scan in a 82 year-old man shows asymmetry of the right vocal cord with thickening due to an irregular lesion, in the middle and anterior third of the vocal cord that infiltrates the anterior commissure and anterior third of the left vocal cord and right subglottis Dx: well-differentiated squamous cell carcinoma in right transglottic T1b2 subglottic involvement Fig 6: Treatment: radical radiotherapy . One week after radiotherapy. Diffuse thickening of the supraglottic mucosal space.
Fig 6: Treatment: radical radiotherapy . One week after radiotherapy. Diffuse thickening of the supraglottic mucosal space.
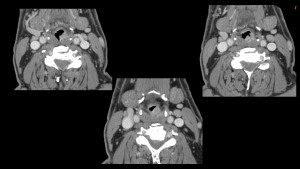
See (Fig 7) : Supraglottic Squamous cell carcinoma after radical radiotherapy.

See (Fig 8-9): Moderately differentiated, invasive Squamous cell carcinoma T3N2M0 and (Fig 10) Post radical radiotherapy.

The lesions most suitable for conservative laryngeal surgery are those that, because of their local invasiveness or proximity to cartilage, are not readily curable with radiation but are small enough to allow adequate resection without sacrificing the entire larynx. Partial laryngectomy also may be a safe and effective treatment for selected cases of recurrent or persistent early- stage cancer that has proved refractory to primary radiation therapy.
- Total (radical) laryngectomy, particularly for advanced (T3-T4 or N+) stages/subglottic tumors, may be held in reserve as a last option for salvage.
Partial laryngectomy techniques
- Endoscopic Laser: Surgery and CordectomyIf a laryngeal cancer is unilateral, is limited to the true vocal cord, and does not impair cord mobility, endoscopic surgery with the use of a carbon dioxide laser for excision is preferred over open surgical approaches such as midline thyrotomy with cordectomy. Only the true vocal cord and the vocalis muscle and tendon are excised.
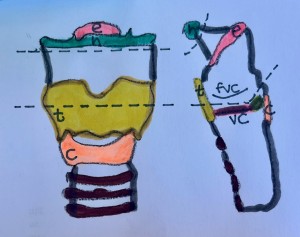
- See (Fig 11): schematic representation of the procedure.
 Fig 11: Axial schematic representation of the procedure: the structures excised (area inside dotted lines) in cordectomy: the true vocal cord (vc), vocalis muscle, and tendon. arytenoid (a), cricoid (c), and thyroid (t) cartilages.
Fig 11: Axial schematic representation of the procedure: the structures excised (area inside dotted lines) in cordectomy: the true vocal cord (vc), vocalis muscle, and tendon. arytenoid (a), cricoid (c), and thyroid (t) cartilages.
After surgery the cord re-generates, and subsequent CT scans show no abnormalities.
See (Fig 12): Squamous cell carcinoma of the right vocal cord T1N0M0 and Post-cordectomy.
- Vertical Partial Laryngectomy: For treatment of early-stage glottic cancers that involve the vocal cord and extend as far as the anterior commissure or the arytenoid cartilage. The two main surgical approaches are frontolateral partial laryngectomy and hemilaryngectomy.
See (Fig.13-14) Supraglottic Squamous cell carcinoma (left aryepiglottic fold ) T2N0M0.
See (Fig 15): Schematic representation of the procedure.

-Frontolateral Laryngectomy:
See summary table. (Table 4).

-Hemilaryngectomy
Indications: unilateral glottic tumors (T1-T2) without invasion of the thyroid cartilage or fixation of the vocal cord.
Surgical procedure: removal of one true vocal cord, part of the ventricle, part of the thyroid cartilage, and possibly the false vocal cord, while preserving the contralateral laryngeal structures.
Expected CT findings:
- Asymmetry of the larynx due to unilateral tissue loss.
- Air or soft tissue in the surgical site.
- Deviation of the airway toward the resected side.
- Fibrosis and soft tissue thickening in the surgical bed.
Key Points to Avoid Misdiagnosis:
- Postoperative fibrosis and scarring are homogeneous and do not grow over time.
- Recurrence appears as an irregular, progressively enlarging, enhancing soft tissue mass that distorts the surgical site.
- Horizontal Laryngectomy: used for treating laryngeal carcinomas are supraglottic laryngectomy and supracricoid laryngectomy.
See (Fig 17): schematic representation of the procedure.
-Supraglottic Laryngectomy:
Indications: for tumors confined to the supraglottis (epiglottis, false vocal cords, and aryepiglottic folds) without extension to the glottis or subglottis. Patients must have preserved vocal cord mobility and no invasion of the paraglottic space or thyroid cartilage.
Surgical procedure: removal of the epiglottis, aryepiglottic folds, false vocal cords, and pre-epiglottic fat, while preserving the glottis and true vocal cords.
Expected CT findings:
- Absence of the epiglottis and pre-epiglottic fat.
- Retraction of the base of the tongue due to fibrosis.
- Enlargement of the supraglottic airway.
How to differentiate from tumor recurrence:
•Postoperative fibrosis appears as stable, homogeneous soft tissue thickening without significant contrast enhancement.
•Recurrence usually presents as a new, irregular, enhancing mass within the surgical bed, often associated with progressive soft tissue thickening.
See (Fig 18): Post supraglottic laryngectomy changes.
-Supracricoid Laryngectomy.
Indications: for glottic or supraglottic tumors without cricoid cartilage invasion, particularly when arytenoid function is preserved.
Surgical procedure: removal of the supraglottis, glottis, and part of the cricoid cartilage, while preserving the hyoid bone and cricoarytenoid unit to maintain phonation and swallowing function.
Expected CT findings:
- Absence of supraglottic and glottic structures.
- Enlargement of the hypopharyngeal airway.
- Postoperative soft tissue thickening in the paraglottic spaces.
- Persistent arytenoid edema in early postoperative imaging.
Key Points to Avoid Misdiagnosis:
- Postoperative edema is expected in the first 6 months, but it should gradually resolve.
- Recurrence is suspected when thickening persists, enhances heterogeneously, and increases in size over time.
Total laryngectomy
Total (radical) laryngectomy, particularly for advanced (T3-T4 or N+) stages/subglottic tumors, may be held in reserve as a last option for salvage.
Normal Postoperative CT Findings See Table 5 
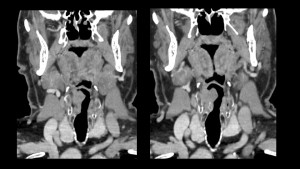
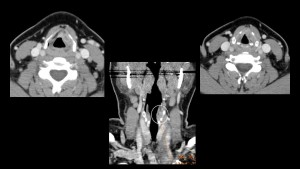
See (Fig 19): Supraglottic Squamous cell carcinoma T4N0M0 and (Fig 20) post-total laryngectomy and (Fig 21) Coronal CT pre-post surgical.



Common Postoperative Complications on CT
1. Pharyngocutaneous Fistula
2. Infection and Abscess Formation. See (Fig. 22).

3. Pharyngeal Stricture See (Fig. 23) Larynx squamous cell carcinoma T3N0M0 and (Fig.24- 25) Post Treatment.


4. Tumor Recurrence
5. Tracheoesophageal Voice Prosthesis-Related Complications
Key Imaging Features to Differentiate Postoperative Changes from Tumor Recurrence Expected Post-Surgical CT Changes:
1. Soft tissue fibrosis and scarring that remain stable over time.
2. Asymmetry of the larynx due to surgical resection, but without progressive distortion.
3. Mild mucosal enhancement, especially in the early postoperative period.
Imaging Features Suggestive of Tumor Recurrence. See Table 6 
Practical Approach to Postoperative Imaging
1. Baseline CT (3-6 months post-surgery): Establishes a reference for future comparisons.
2. Serial CT Scans (Every 3-6 months for the first 2 years): Helps assess stability or progression.
3. PET-CT for indeterminate cases: Differentiates fibrosis from recurrence based on metabolic activity.
4. Biopsy if suspicious findings are present: Persistent, progressively enhancing lesions should be evaluated further.