Anatomy and normal variants
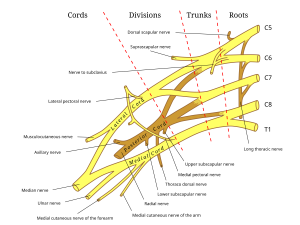
The brachial plexus is a network of nerves that originates from the ventral rami of the C5 to T1 spinal nerves. These roots combine to form three trunks: the upper (C5-C6), middle (C7), and lower trunk (C8-T1). Each trunk divides into an anterior and posterior division, which merge to form three cords: the lateral, posterior, and medial cords. The cords give rise to the terminal branches, which include the musculocutaneous, axillary, radial, median, and ulnar nerve. They are responsible for motor and sensory innervation of the upper limb. Passage of the C5 and C6 root through or anterior to the anterior scalene muscle is one of the most common brachial plexus variants.The prefixed brachial plexus is an anatomical variant, where the roots of the brachial plexus arise from C4-C7 instead of C5-T1. In the postfixed brachial plexus, the roots arise from C6-T2. Both of these variants can alter the braching pattern of the nerves and may even affect the nerve innervation of the upper limb.
Common pathologies
Traumatic brachial plexus injury
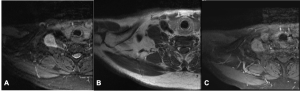
Traumatic brachial plexus injuries are often caused by high-energy traumas such as motor vehicle accidents or sports injuries, leading to damage of the nerve roots or trunks. The most common trauma mechanism is excessive stretching of the plexus. Depending on the severity of the injury, symptoms range from weakness and numbness to paralysis of the affected arm. Brachial plexus injuries are classified based on the severity and location of the damage. A commonly used classification is the Sunderland classification, which focuses on the degree of the nerve damage and categorizes the brachial plexus injuries into five degrees. MRI is a valuable tool for assessing brachial plexus injuries and is particularly helpful in distinguishing between different types of nerve damage such as avulsion (nerve root is torn from the spinal cord) and rupture (nerve torn, but not from the spinal cord). MRI also visualizes hematomas, neuromas and soft tissue injuries.
Thoracic outlet syndrome (TOS)
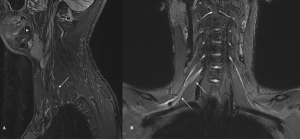
TOS is a condition, where the compression of the neurovascular structures at the thoracic outlet (the space between the collarbone and the first rib) leads to symptoms such as pain, numbness, paresthesia and weakness. The neurogenic form of TOS - caused by compression of the brachial plexus - is the most common form (> 90%). Common risk factors include anatomical variations (for example a cervical rib), previous trauma or surgery, repetitive overhead activities, scalene muscle hypertrophy and obesity. TOS is more common in women than men. MRI helps diagnose the underlying causes of TOS, particularly in cases where structural abnormalities such as a cervical rib, an abnormal first rib or scalene muscle hypertrophy are involved.
Parsonage-Turner syndrome (PTS) - an inflammatory plexopathy
PTS, also known as idiopathic brachial plexitis, is a rare inflammatory, self-limited brachial neuritis that affects the brachial plexus, leading to sudden-onset pain followed by muscle weakness and atrophy in the shoulder and upper arm. The exact cause is unclear, but PTS is often associated with viral infections, vaccinations (diphtheria-tetanus-pertussis or influenza), trauma, or autoimmune disorders (e.g. rheumatoid arthritis or systemic lupus erythematosus). PTS is diagnosed based on the combination of clinical presentation and imaging. MRI helps to identify the inflammatory nature of the disease while excluding structural lesions. MRI features of PTS include brachial plexus edema and enhancement, nerve root enlargement (especially C5 and C6) and muscle atrophy and fatty infiltration (most commonly supra- and infraspinatus muscle followed by deltoid).
Infectious plexus neuritis
Infectious plexus neuritis is an inflammation of the brachial plexus typically caused by viral or bacterial infections. Common pathogens include herpes simplex virus, varicella-zoster virus and Epstein-Barr virus. Bacterial pathogens such as Borrelia burgdoferi or Mycobacterium tuberculosis are less frequently involved. Clinically, infectious plexus neuritis presents with pain, weakness and sensory deficits in the affected arm. On MRI, infectious plexus neuritis typically shows enlargement, T2-weighted hyperintensity and contrast enhancement of the affected brachial plexus roots and trunks.
Neoplastic involvement of the brachial plexus
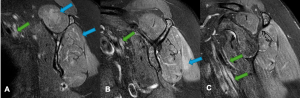
Tumorous conditions affecting the brachial plexus might be symptomless in the early stages of the disease and discovered incidentally. As they grow, brachial plexus tumors lead to pain, muscle weakness and paresthesia. Common primary tumors of the brachial plexus include nerve sheath tumors such as schwannomas, neurofibromas and malignant peripheral nerve sheath tumors. Schwannoma and neurofibroma are iso- oder hypointens on T1-weighted imaging and mostly hyperintens on T2-weighted imaging. Both may show a “target sign”, meaning a central hypointensity surrounded by peripheral hyperintensity on T2-weighted imaging. Malignant peripheral nerve sheath tumors are larger than benign nerve sheath tumors and show a more invasive growth pattern. Secondary tumors affecting the brachial plexus include Pancoast tumors, breast cancer and breast cancer metastases as well as lymphoma.