In suspected cases of NPH:
-Rule out obstructive hydrocephalus.
-Assess patient history for previous cerebral hemorrhages, meningitis, encephalitis, tumors, surgeries, or any condition that may affect CSF absorption.
Imaging Analysis:
- CT scan: First-line imaging tool providing an initial diagnostic impression.
- MRI: Superior for detecting morphological changes.
Radiological findings:
Imaging findings reflect the brain´s response to impaired CSF absorption:
-Increased vascular pulsatility displaces neural tissue around blood vessels, particularly in the Sylvian fissures.
-Ventriculomegaly occurs due to systolic pressure peaks, exerting force on the ventricular walls, especially at the frontal horns of the lateral ventricles.
-Increased CSF flow velocity is more evident in narrow regions of the ventricular system, particularly in the aqueduct of Sylvius.
Key Imaging Features Suggestive of NPH:
- Ventriculomegaly: Enlargement of the lateral and third ventricles, with relative sparing of the fourth ventricle. Indices used for assessment:
 Fig 1: Ventriculomegaly. Non-contrast axial CT scan of the brain. Dilation of the lateral ventricles (orange arrows) and the third ventricle (red arrow), consistent with ventriculomegaly. (Radiology Department. Complejo Asistencial de Zamora).
Fig 1: Ventriculomegaly. Non-contrast axial CT scan of the brain. Dilation of the lateral ventricles (orange arrows) and the third ventricle (red arrow), consistent with ventriculomegaly. (Radiology Department. Complejo Asistencial de Zamora).
-Evans' Index: Estimates ventricular volume using the ratio between the maximum width of the frontal horns of the lateral ventricles and the biparietal diameter of the skull on axial CT/MRI images.
Interpretation:
- 20–0.25: Normal
- 25–0.30: Mild ventriculomegaly
- >0.30: Ventriculomegaly
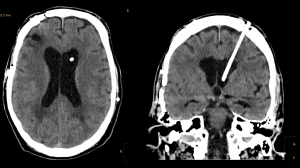
 Fig 2: Evans´ index. Non-contrast axial CT scan of the brain (left) and axial T2 FLAIR-weighted brain MRI (right). Dilation of the lateral ventricles with an Evans' index of 0.39. Findings suggestive of ventriculomegaly. (Radiology Department. Complejo Asistencial de Zamora).
Fig 2: Evans´ index. Non-contrast axial CT scan of the brain (left) and axial T2 FLAIR-weighted brain MRI (right). Dilation of the lateral ventricles with an Evans' index of 0.39. Findings suggestive of ventriculomegaly. (Radiology Department. Complejo Asistencial de Zamora).
-Anteroposterior Lateral Ventricle Index (ALVI): Proposed by Wenji He et al. (2020), the index is not yet widely adopted but considered more reproducible and faster than Evans' index. Is it measured using axial images, selecting the most caudal slice where the entire lateral ventricle body is visible without thalamic obscuration. ALVI calculates ventricular size using the ratio between the anteroposterior diameter of the lateral ventricle and the anteroposterior skull diameter at the same level.
Interpretation:
- <0.5: Normal
- >0.5: Ventriculomegaly
 Fig 3: ALVI. Non-contrast axial CT scan of the brain (left) and axial T2 FLAIR-weighted brain MRI (right). Dilation of the lateral ventricles, with an ALVI of 0.56 and 0.61, respectively. Findings suggestive of ventriculomegaly. (Radiology Department. Complejo Asistencial de Zamora).
Fig 3: ALVI. Non-contrast axial CT scan of the brain (left) and axial T2 FLAIR-weighted brain MRI (right). Dilation of the lateral ventricles, with an ALVI of 0.56 and 0.61, respectively. Findings suggestive of ventriculomegaly. (Radiology Department. Complejo Asistencial de Zamora).
- Temporal horn enlargement >6 mm, not attributable to hippocampal atrophy.
- Acute callosal angle: More predictive than traditional indices, with prognostic value: a sharper the angle correlates with better response to VPS.
Interpretation:
- Normal: 100º-120º
- NPH: <90º.
 Fig 4: Normal callosal angle. Coronal T1-weighted brain MRI. Callosal angle within normal limits (115º) (Radiology Department. Complejo Asistencial de Zamora).
Fig 4: Normal callosal angle. Coronal T1-weighted brain MRI. Callosal angle within normal limits (115º) (Radiology Department. Complejo Asistencial de Zamora).
- Periventricular white matter changes, particularly around the frontal horns and ventricular atria, caused by CSF leakage into the brain parenchyma due to systolic pressure peaks. This leads to gliosis and periventricular ischemia ("transependymal edema"). MRI is more sensitive than CT for detecting these alterations.
 Fig 5: Periventricular white matter changes. Non-contrast axial CT scan of the brain (left) and axial T2 FLAIR-weighted brain MRI (right). Areas of gliosis and periventricular ischemia around the frontal horns of the lateral ventricles (red arrows) and the ventricular atria (orange arrows), suggestive of transependymal edema. (Radiology Department. Complejo Asistencial de Zamora).
Fig 5: Periventricular white matter changes. Non-contrast axial CT scan of the brain (left) and axial T2 FLAIR-weighted brain MRI (right). Areas of gliosis and periventricular ischemia around the frontal horns of the lateral ventricles (red arrows) and the ventricular atria (orange arrows), suggestive of transependymal edema. (Radiology Department. Complejo Asistencial de Zamora). - Sylvian fissure and insular widening, disproportionate to the narrowing of other cortical sulci. This is attributed to increased perivascular pressure in vessels dependent on the middle cerebral artery.
 Fig 6: Widening of Sylvian fissures. Non-contrast coronal CT scan of the brain (left) and coronal T2-weighted brain MRI (right). Widening of both Sylvian fissures (red arrows) disproportionate to the narrowing of other cortical sulci. (Radiology Department. Complejo Asistencial de Zamora).
Fig 6: Widening of Sylvian fissures. Non-contrast coronal CT scan of the brain (left) and coronal T2-weighted brain MRI (right). Widening of both Sylvian fissures (red arrows) disproportionate to the narrowing of other cortical sulci. (Radiology Department. Complejo Asistencial de Zamora). - Marginal callosal sulcus sign: The posterior half of the cingulate sulcus is narrower than the anterior half.
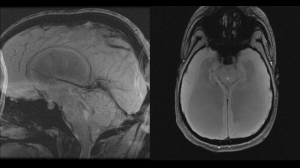
 Fig 7: Marginal callosal sulcus sign. Sagittal T2-weighted brain MRI. The posterior half of the cingulate sulcus is narrower than the anterior half (red arrow). (Radiology Department. Complejo Asistencial de Zamora).
Fig 7: Marginal callosal sulcus sign. Sagittal T2-weighted brain MRI. The posterior half of the cingulate sulcus is narrower than the anterior half (red arrow). (Radiology Department. Complejo Asistencial de Zamora). - Bulging of the corpus callosum.
 Fig 8: Bulging of the corpus callosum. Sagittal T1-weighted brain MRI. Thinning (red arrow) and bulging (orange arrow) of the corpus callosum. (Radiology Department. Complejo Asistencial de Zamora).
Fig 8: Bulging of the corpus callosum. Sagittal T1-weighted brain MRI. Thinning (red arrow) and bulging (orange arrow) of the corpus callosum. (Radiology Department. Complejo Asistencial de Zamora). - Bulging of the lamina terminalis of the third ventricle and the infundibular recess.
 Fig 9: Bulging of the terminal lamina of the third ventricle and the infundibular recess. Sagittal T2-weighted brain MRI. Bulging of the terminal lamina of the third ventricle and the infundibular recess (red arrow). (Radiology Department. Complejo Asistencial de Zamora).
Fig 9: Bulging of the terminal lamina of the third ventricle and the infundibular recess. Sagittal T2-weighted brain MRI. Bulging of the terminal lamina of the third ventricle and the infundibular recess (red arrow). (Radiology Department. Complejo Asistencial de Zamora). - Effacement of cortical sulci, particularly at the vertex and parasagittal regions.
- Focal or isolated enlargement of individual convexity sulci.
Phase-Contrast MRI for CSF Flow Analysis
Phase-contrast MRI sequences can assess CSF flow qualitatively and quantitatively. In NPH, a flow void in the aqueduct of Sylvius is commonly observed due to increased CSF velocity. However, the absence of CSF flow in the aqueduct can also be seen in healthy individuals.
Key CSF Flow Findings in Phase-Contrast MRI for NPH Diagnosis and Prognosis:
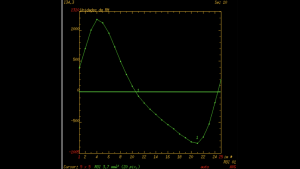
-Increased Systolic CSF Stroke Volume: This refers to the average volume of CSF flowing through the aqueduct during systole and diastole. In advanced stages of NPH, the stroke volume paradoxically decreases due to cerebral atrophy, sugesting a poor response to VP shunting.
-Elevated Peak Flow Velocity in the Aqueduct: The upper limit is typically twice the normal value. Higher flow velocities are associated with a better prognosis post VPS.
-Increased Slope and Narrowing of Velocity-Time Curves: In NPH, the velocity-time curve demostrates a narrower systolic phase with a steep descending slope, which is indicative of NPH.
Treatment and Prognosis:
The primary treatment for NPH is ventriculoperitoneal shunt. Favorable prognostic factors include:
-A short duration of preoperative symptoms (less than 6 months).
-Gait disturbance preceding cognitive decline.
-Symptomatic relief after lumbar puncture, demonstrated by a 40 mL CSF tap test.
-Absence of significant cerebrovascular disease.
-Presence of a CSF flow void and high CSF flow velocities in qualitative and quantitative CSF studies.