Anatomy
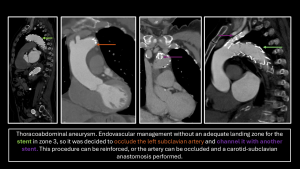
The aorta is subdivided into various zones; the most widely accepted classification is that of Criado and Ishimaru, which divides it into 9 zones: the thoracic aorta (zones 0–5) and the abdominal aorta (zones 6–9). This classification is the most commonly used in the surgical field. In this article, our focus is on zones 0–4.
- Zone 0: Aortic root and ascending aorta, including the origin of the innominate artery.
- Zone 1: Area that includes the origin of the left common carotid artery.
- Zone 2: Area that includes the origin of the left subclavian artery.
- Zone 3: From the distal aspect of the left subclavian artery to the first 2 cm of the descending aorta.
- Zone 4: Extends distally along the descending aorta.
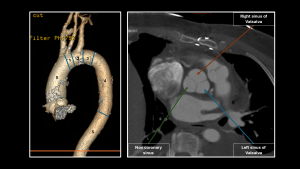
The aortic root is a complex region of the aorta that separates the left ventricle from the systemic circulation. It extends from the aortic annulus (the fibrous support of the aortic valve) to the sinotubular junction (where the valve cusps join the aortic wall). It includes the Valsalva sinuses: the right coronary artery originates from the right sinus, the left coronary artery from the left sinus, and the non-coronary sinus is located posteriorly and does not give rise to any artery.

What pathologies lead to surgical repair of the aorta?
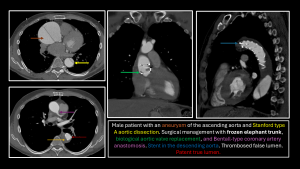
All conditions included in acute aortic syndrome (aortic dissection, intramural hematoma, limited intimal tear, penetrating atherosclerotic ulcer, or a leaking/ruptured aortic aneurysm). Among the risk factors for these pathologies are history of Marfan syndrome, bicuspid aortic valve, Ehlers-Danlos syndrome and Loeys-Dietz syndrome.
How is the aorta repaired?
- Zone 0 (aortic root and ascending thoracic aorta): Surgical replacement using composite grafts (Bentall or Cabrol techniques) or valve-sparing techniques (David, Yacoub).
- Zones 1–4 (aortic arch): Hybrid techniques (surgical + endovascular) or open surgical repair.
Which exam is indicated to evaluate patients in the postoperative period after thoracic aorta reconstruction?
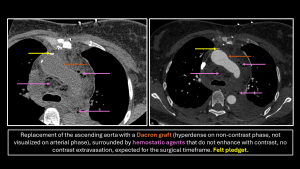
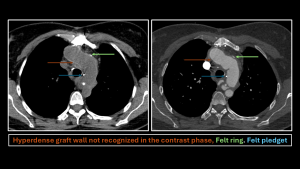
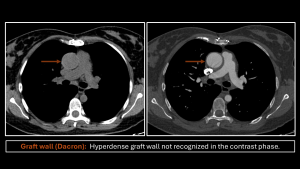
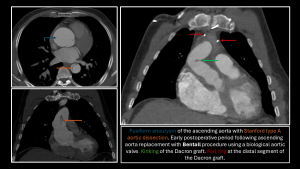
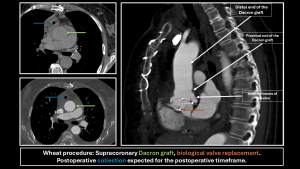
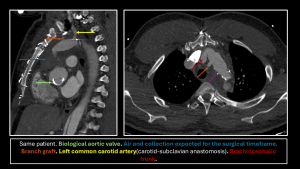
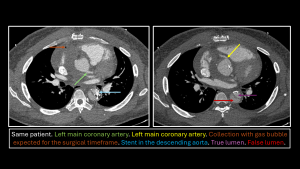
It is recommended to perform a chest CT angiography in both non-contrast and arterial phases, ideally synchronized with ECG. The non-contrast phase is crucial in the postoperative setting, as it allows the identification of surgical materials—which are slightly hyperdense and may be obscured in the contrast-enhanced phase.
How to identify a graft on CT?
Grafts present with a nonanatomic appearance, generally appearing straighter with sharp angulations at the anastomosis sites. On non-contrast CT, they are hyperdense compared to the native aortic wall, whereas in the arterial phase they may be less conspicuous due to contrast enhancement. Other elements, such as felt reinforcement rings, sutures, and metallic clips, help delineate the margins of the graft and confirm its location. They can be confused with circumferential calcifications or, in patients with anemia, with blood that appears hypodense compared to the wall.
What does the proper interpretation of postoperative aortic CT angiography depend on?
- Understanding the surgical repair techniques that are performed
- Identifying key points to consider
- Recognizing the normal post-surgical appearance, such as perigraft fluid or transient mediastinal air.
- Recognizing, by imaging, the commonly used repair components
- Felt rings
- Felt patches
- Surgical sutures
- Surgical clips
What key points should we consider?
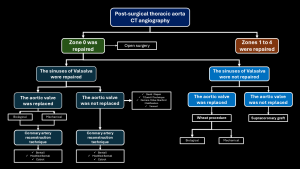
- Repairs of the Ascending Aorta (Zone 0)
- Determine whether the aortic valve has been repaired:
- Mechanical.
- Bioprosthetic: valve leaflets are not visualized; instead, the metallic framework is seen.
- Determine whether the Valsalva sinuses have been repaired.
- Supracoronary (Wheat technique).
- Replacement of the Valsalva sinuses (with reimplantation of the coronary arteries).
- Techniques that replace the native valve: Bentall or Cabrol.
- Techniques that preserve the native valve: Yacoub or David.
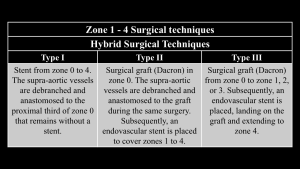
- Repairs Involving the Aortic Arch (Zones 1–4)
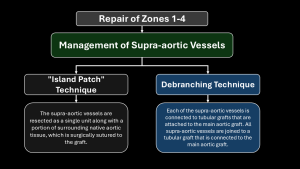
- Management of the supra-aortic vessels.
- Distal extension of the repair.
How is the thoracic aorta repaired: Zone 0?
Synthetic grafts (Dacron) or human donor grafts (rarely used) are utilized. In the past, the inclusion technique was employed, in which the native aorta was sutured around the graft, creating a space that could accumulate fluid or blood. Today, the interposition technique—where the diseased aorta is replaced with a graft—is preferred.
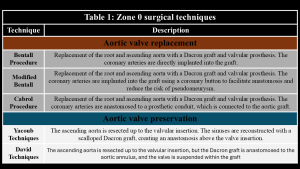
Surgical Techniques:
- Composite valve graft (replaces the aortic valve): Bentall or Cabrol.
- Aortic root graft with valve preservation: Yacoub or David.
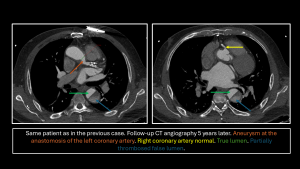
Composite Valve Graft: This technique is used in aneurysms or dissections of the aortic root and ascending aorta. The valve is replaced with mechanical prostheses (necessitating lifelong anticoagulation) or biological prostheses (with a risk of degeneration). Complications include leakage at the anastomosis, coronary artery pseudoaneurysm (>10 mm), or thrombosis of the coronary graft.
- Bentall Technique (1968): Replacement of the aortic root and ascending aorta with a valvular prosthesis and proximal graft, with direct reimplantation of the coronary arteries.
- Modified Bentall: Includes a coronary button to facilitate the anastomosis and reduce the risk of pseudoaneurysm.
- Cabrol Technique (1981): An alternative to the Bentall procedure. The coronary arteries are anastomosed to a prosthetic conduit, which is then connected to the aortic graft. This technique is useful in patients with post-surgical changes, proximal coronary disease, or coronaries that are difficult to mobilize.
- Wheat Procedure (1964): Supracoronary ascending aortic graft and valve replacement while preserving the Valsalva sinuses. Complications include dissection or aneurysm proximal to the graft.
Aortic Root Repair Surgery with Valve Preservation: Indicated in patients with a healthy aortic valve to avoid complications associated with prosthetic valves and long-term anticoagulation. The main complication is aortic valve insufficiency.
- Yacoub Technique (Remodeling): Described in 1980. It involves resecting the native aorta up to the valve insertion, with the sinuses being reconstructed using a scalloped Dacron graft to create an anastomosis above the valve insertion.
- David Technique (Reimplantation): Similar to the Yacoub technique, but the Dacron graft is anastomosed to the aortic annulus and the valve is resuspended within the graft.
- David-V (Stanford Modification): Uses two grafts to adjust the dimensions of the aortic root and reconstruct the ascending aorta, thereby recreating the Valsalva sinuses.
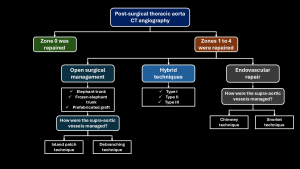
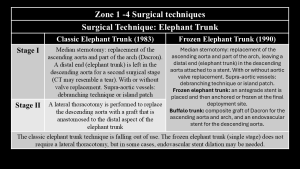
How is the aorta repaired: Zones 1–4?
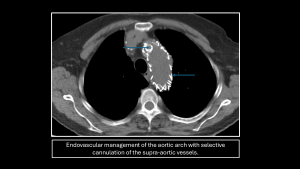
The repair can be surgical, endovascular, or hybrid, and may be combined with repairs of the ascending or descending aorta. The method used to reconstruct the supra-aortic vessels is the most important aspect.
- Surgical: Elephant trunk technique or prefabricated grafts, managing the supra-aortic vessels with the "island patch" technique or debranching.
- Endovascular: Customized stents tailored to the supra-aortic vessels using chimney or snorkel techniques.
- Hybrid: Three subtypes.

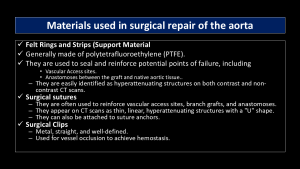
What surgical materials are used and observed in postoperative CT angiography?
During aortic repairs, polytetrafluoroethylene (PTFE) rings and patches are used to reinforce anastomoses and seal critical points, appearing on CT as hyperattenuating structures. Surgical sutures reinforce vascular access sites, grafts, and anastomoses, and they appear on CT as thin hyperattenuating lines or hook-shaped structures. Surgical clips, used to control bleeding, are identified as straight metallic structures. Endovascular stents, with a nitinol metallic framework, may include fenestrations or branches for the supra-aortic vessels; their internal framework is visible on CT as hyperdense struts.
What are the main complications in these surgical procedures?
- Graft rupture.
- Anastomotic dehiscence.
- Infection.
- Pseudoaneurysms.
- Endoleaks.
- Stent thrombosis.
It is important to identify changes in the graft contour, increasing perigraft fluid (or fluid with mild enhancement), vascular irregularities, or new or increasing perigraft air (which is expected up to one week following reconstruction).
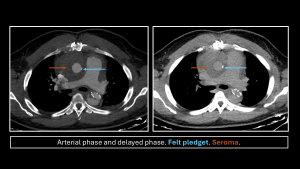
What mistakes can be made when interpreting a postoperative aortic ct angiography?
- Bioabsorbable hemostatic agents:
- They are absorbed within 7–14 days (longer if a large quantity is used).
- They can mimic abscess, hematoma, or foreign bodies (presenting as heterogeneous masses with gas and mild enhancement).
- Differentiation: Look for linear gas bubbles that remain unchanged, without an air–fluid level or wall enhancement.
- Graft folds:
- These can mimic a dissection flap.
- Lateral branch grafts:
- Used for cannulation and perfusion; they are closed at the end with suture, felt, or clips. If not identified, they may resemble pseudoaneurysms.