I. RESULTS
- Epidemiological Characteristics of NSCLC Brain Metastases in Our Institution
Among 80 suspected cases of brain metastases, 74 patients were confirmed to have brain involvement, of which 67 had NSCLC.
- Histological Subtypes:
- 57 adenocarcinomas (ADK)
- 5 squamous cell carcinomas (SCC)
- 2 sarcomatoid carcinomas
- 2 non-specified NSCLC
- 1 missing data
- Demographics:
- Mean age: 62.3 years
- Male: 55, Female: 12
- Strong smoking association
- Mode of Metastasis Detection:
- Systematic extension workup in known lung cancer cases.
- Neurological symptoms such as headaches, visual disturbances, gait abnormalities, balance disorders, focal neurological deficits, or signs of intracranial hypertension.
- Incidentally detected in rare cases.
- Treatment:
- Predominantly radiotherapy.
- Stereotactic radiosurgery (SRS) for oligometastatic cases.
- Whole-brain radiotherapy (WBRT) for multiple metastases.
- Surgical resection in 3 cases with single accessible lesions.
2. Imaging Characteristics of NSCLC Brain Metastases
- Lesion Count:
- 34 cases presented a single metastasis.
- 15 cases had 2–3 lesions.
- 5 cases had 4–5 lesions.
- 13 cases exhibited multiple (>5) lesions.
- Location:
- 40 cases were exclusively supratentorial.
- 21 cases had both supra- and infratentorial involvement.
- 6 cases were purely infratentorial.
- One patient demonstrated a leptomeningeal localisation.
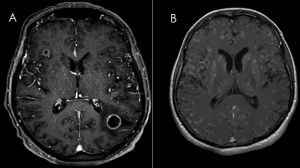
- Morphological MRI characteristics :
- Parenchymal: Most lesions were intraparenchymal cystic or cystic-solid : 52 cases displayed cystic or cystic-solid characteristics. 15 cases were purely solid.
- Most lesions (85%) exhibited ring enhancement with a mural nodule in some cases.
- Hypointense on T1-weighted imaging and Hyperintense on T2 and FLAIR sequences in all patients.
- Lesions ranged in size from 3 mm to several centimeters.
- Peritumoral edema was present in all patients, significant in most cases.
- 4 cases were associated with hydrocephalus.
- 6 cases showed brain herniation.
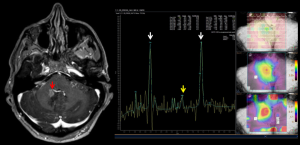
- Multiparametric MRI Characteristics:
- SWI sequence showed no hemorrhagic components in most cases, except in 4 patients.
- ADC values were elevated, reflecting high extracellular water content.
- PWI (T2* DSC-MRI) demonstrated increased relative cerebral blood volume (rCBV) in metastases.
- MRS sequences revealed choline peaks and low NAA, helping distinguish these metastases from gliomas and abscesses.
II. DISCUSSION
A. Epidemiology
- Solid tumors most commonly associated with brain metastases.
- Approximately 9% to 17% of brain metastases (BM) are diagnosed at initial cancer presentation.
- Recent studies report BM rates of up to 38% at diagnosis, particularly in patients with ALK rearrangement.
- Brain metastases develop in 40% to 50% of cases during follow-up.
- Classically, BM are more frequent in adenocarcinomas than in squamous cell carcinomas. (1)
B. Clinical presentation
- Asymptomatic (Silent Metastases): 60–75% of cases
- Symptomatic Presentations:
- Headaches: 70%
- Seizures: 62%
- Focal neurological deficits: 58%
- Signs of intracranial hypertension: 33%
- Cognitive impairment, visual disturbances, memory deficits, and confusion may also occur. (2)
C. Imaging Modalities
- Computed tomography CT scan
- First-line imaging modality.
- Remains essential in the diagnostic process.
- Rapid, widely available, and often sufficient for diagnosis.
- Typical features highly suggestive of brain metastases (BM):
- Hypodense lesions on non-contrast CT.
- Possible spontaneous hyperdensity in hemorrhagic metastases.
- Contrast enhancement: nodular, ring-enhancing, or diffuse.
- Significant vasogenic perilesional edema, often disproportionate to tumor size.
- Magnetic Resonance Imaging (MRI)
- Gold standard for detection and characterization of brain metastases.
- Higher sensitivity than CT, especially for detecting small or multiple lesions.
- Essential for treatment planning (surgery, stereotactic radiosurgery).
- Positron Emission Tomography (PET-CT)
- Used for whole-body evaluation to identify the primary tumor and other metastatic sites.
- Can be helpful in differentiating tumor recurrence from radiation necrosis. (2)
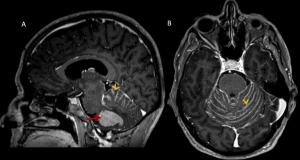
D. Different figures of brain metastasis from lung cancer
- Location:
- Parenchymal (most common)
- Dural-based: Rare cases mimicked meningiomas. (3)
- Leptomeningeal carcinomatosis: Identified in diffuse cases, best visualized on contrast-enhanced FLAIR sequences. (4)
- Choroid plexus & pineal metastases: Rare but observed in highly vascularized variants.
- Number: Unique or multiple
- Enhancing Feature: Annular or nodular (2)
E. Places of Advanced Imaging Features
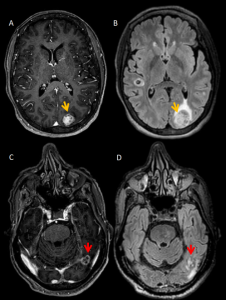
- Diffusion Weighted Imaging :
- Assess Tumor Cellularity: DWI can reflect tumor cellularity, with higher cellularity often leading to restricted diffusion and lower apparent diffusion coefficient (ADC) values.
- Brain metastases typically show restricted diffusion at the enhancing rim due to hypercellularity, with relatively high ADC values in the central necrotic zone.
- DWI is crucial in distinguishing ring-enhancing brain metastases from pyogenic abscesses, a common diagnostic challenge. (5)
- Perfusion Imaging (T2* and ASL):
-
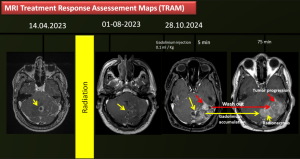
Perfusion-Weighted Imaging (PWI), particularly T2*-based Dynamic Susceptibility Contrast MRI (DSC-MRI), plays a crucial role in assessing brain metastases. It demonstrates increased relative cerebral blood volume (rCBV) in metastatic lesions, aiding differentiation from radiation necrosis, which typically exhibits low rCBV. Arterial Spin Labeling (ASL) perfusion further confirms hyperperfusion in active metastases, offering valuable information without contrast administration, especially in cases of tumor hemorrhage.
-
Clinically, PWI is used to monitor perfusion changes following stereotactic radiotherapy (SRT). A significant post-treatment reduction in rCBV often correlates with a favorable response, whereas stable or increased rCBV may indicate tumor progression. Despite limitations such as small lesion size and susceptibility artifacts, PWI remains an essential tool for assessing brain metastases in NSCLC, guiding treatment decisions and monitoring therapeutic efficacy. (6)
- Magnetic Resonance Spectroscopy (MRS):
- Magnetic Resonance Spectroscopy (MRS) is a non-invasive imaging technique that provides metabolic information about brain tissues, complementing traditional MRI by detecting biochemical changes associated with tumors. In the context of brain metastases from non-small cell lung cancer (NSCLC), MRS has several clinical applications:
- Differentiation of Lesion Types: MRS aids in distinguishing between metastatic tumors and other intracranial lesions, such as abscesses or radiation-induced necrosis. Metastatic lesions often exhibit elevated choline (Cho) levels due to increased membrane turnover, while abscesses show different metabolic profiles. This differentiation is crucial for determining appropriate treatment strategies.
- Prognostic Assessment: Quantitative MRS parameters, particularly the choline-to-creatine (Cho/Cr) ratio, have been linked to patient outcomes. Higher Cho/Cr ratios in brain metastases have been associated with poorer overall survival and progression-free survival in NSCLC patients undergoing stereotactic radiotherapy. This suggests that MRS can provide prognostic information, potentially guiding therapeutic decisions.
- Monitoring Treatment Response: MRS can detect metabolic changes in tumors following therapy before structural changes become apparent on conventional MRI. A decrease in Cho levels post-treatment may indicate a positive response, whereas stable or increased levels could suggest treatment resistance or tumor progression. This early detection capability allows for timely adjustments in therapeutic approaches. (7)
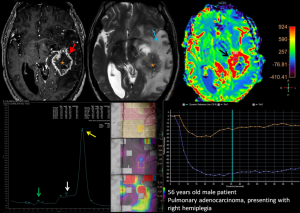
- TRAM (Treatment response assessement mapping) = T1-weighted gradient echo with arterial input function mapping, a promising sequence that enhances perfusion assessment and provides additional contrast kinetics data to differentiate active tumor regions from treatment effects.
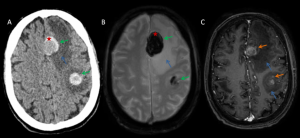
F. Differential Diagnosis of NSCLC Brain Metastases
- Gliomas: Usually infiltrative with ill-defined margins and demonstrate increased rCBV on perfusion. IDH-mutant gliomas often show lower perfusion compared to metastases.
- Abscesses: Typically display central restricted diffusion on DWI, central low choline on MRS with elevated lactate and lipids, and a smooth thin rim of enhancement.
- Primary CNS Lymphoma: Homogeneously enhancing lesions with restricted diffusion and high cellularity.
- Radiation Necrosis: Low rCBV on perfusion MRI with gadolinium accumulation at 75 min after injection, whereas active metastases show high rCBV and wash out of gadolinium at 75 min after injection.
G. Post-Therapeutic Imaging Changes and Radiation Necrosis
- Radiation necrosis mimics recurrence but exhibits low rCBV on perfusion imaging.
- FDG-PET and advanced MRI sequences like MRS (low choline) help distinguish necrosis from viable tumor.
- TRAM sequence offers additional insights into treatment effects and residual tumor activity.
III. LIMITATIONS
- Retrospective aspect of the study.
- Our department is the referral center for oncology, with a significant number of patients. This has made it challenging to perform advanced imaging sequences for all patients.